May 2022
VOLUME XXXVI, NUMBER 02
MAY 2022, VOLUME XXXVI, NUMBER 02
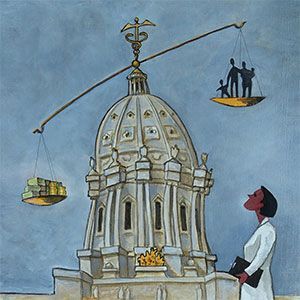
Minnesota health care roundtable
Care Transitions: Improving the safety net
The following report from the 54th session of the Minnesota Health Care Roundtable continued on the theme of our last program, which focused on improving the interoperability of care teams. In this session, we are looking specifically at the topic of care transitions. As the scope of care teams expands, with an increasingly varied number and type of health care providers involved, the opportunity for unintended consequences also expands. Care transitions have become a leading source of malpractice litigation. Our panel discusses these issues and how best to address them. We extend our special thanks to the participants and sponsors for their commitments of time and expertise in bringing you this report. This fall we will publish the 55th session of the Minnesota Health Care Roundtable on the topic Care Coordination. This will complete the exploration of a trilogy of emerging and related responses to the necessary evolution of health care policy. We welcome comments and suggestions.
the panelist
Todd Archbold LSW, MBA after joining PrairieCare in 2006 Todd became chief executive officer in 2020. He has helped develop one of the region’s largest psychiatric health systems with 12 locations in Minnesota. He is also the executive director for the Psychiatric Assistance Line (PAL) – a statewide service aimed towards increasing collaboration and support between psychiatry and primary care.
Bonnie LaPlante, MHA, BS RN is the health care home (HCH) program director, in the Health Policy Division, at the Minnesota Department of Health, where she has worked for over 9 years. She has sixteen years of leadership experience as a clinic services nursing director, as well as experience as a director of a home health agency and a coordinator in long term care.
Lindsey Sand, LHSE, NHA serves as vice president of population health for Knute Nelson, an aging services organization offering a full continuum of services across more than 35 counties in northwestern and central Minne-sota and eastern North Dakota. She serves on the board of Lakes Area Age-Friendly, LeadingAge Minnesota, and the LeadingAge Minnesota Foundation.
David S. Schultz, MD, MHA is the medical director and founder of Nura Pain Clinics. Dr. Schultz is a board-certified anesthesiologist with additional board certification in pain medicine from the American Board of Anesthesiology, the American Board of Interventional Pain Physicians, and the American Board of Pain Medicine. He has been a full-time interventional pain specialist since 1995.
David J. Voller, MBA, FACHE is the clinic administrator at Shriners Children’s Twin Cities. His 30 year career in healthcare and health care includes positions at the Mayo Clinic, Gillette Children’s and BWBR. David is a Fellow of the American College of Healthcare Executives, sits on the board of ACHE MN and chair for membership and advancement.
about the sponsors
Coverys is a medical liability insurance company that combines insurance protection with risk analytic services. They are a national leader in the field with over 45 years experience protecting health care.
LeadingAge Minnesota Foundation supports initiatives to transform and enhance the experience of aging by building the workforce for tomorrow, advancing promising new approaches to service delivery, and developing leadership at all levels.
Nura Pain Clinic was created by physicians who are pioneers in precision pain management. For over three decades they have specialized in therapies and procedures helping those who struggle with chronic pain get their life back.
RAYUS Radiology, formerly CDI, is a nationwide leader in advanced diagnostic and interventional radiology. Blending the art and science of well-being, RAYUS is revolutionizing radiology and making the unknown known for over a million patients and their providers each year.
The term care transition covers a lot of ground. Please tell us what this means from your perspective.
Dr. Schultz: Care transition is a term that describes the process of information exchange when patients move between medical practices. Successful transitioning of patient care from one medical practice to another requires quick, efficient and thorough interchange of health information between medical providers. Interoperable electronic health records were supposed to make the process of information exchange between medical practices seamless, but this has not happened in any consistent manner.
Lindsey: From our perspective, care transitions can be viewed in two ways. It can refer to the transitions of a patient from a hospital to a skilled care facility or even to their home where patients could utilize skilled care, personal care or independent self-management. It can also refer to health status changes. No matter their current care location, the patient may require more extensive care or less intensive service delivery. This type of transition can involve a health status setback on the road to recovery or new development that may require adjustments to the care plan.
Bonnie: Care transition covers a wide spectrum in primary care. Broadly, it means the transfer of care from one setting or level of care to another–for example, from a hospital to home or a residential care facility with return of care to the primary care provider. In certified Health Care Home clinics, transition procedures are developed and used to ensure safety and to prevent health complications, gaps in care and rehospitalization.
David: The definition of care transition really comes with two factors that represent care collaboration and coordination while the patient is in our care, but also the intentionality of what that care will look like when the patient is not in or not longer going to be in our care. This process starts immediately when the patient is presented. This care transition can occur either internally with other providers or externally with referring or primary care providers.
TodD: Care transition is inevitable. It can range from simply changing care providers, moving between levels of care, seeking specialists and discharging from a hospital. Care transition can signal progress in one’s condition, or conversely, it could be the advancement of a disease. It can also be prompted by misdiagnosis or inadequate treatment. In each of the situations, a health system’s ability to effectively manage the transition of care is a critical component to the triple aim and an ethical responsibility of individual care providers.
True interoperability is key to improving care transitions.
—Todd Archbold
What are some of the most common problems that arise from care transitions?
Lindsey: It all boils down to communication and clarity, especially when multiple providers are involved. Often there is a lack of transparency within communications between caregiver groups which becomes problematic for many reasons, not the least of which is everyone wastes time duplicating effort. It is vitally important that there be clarity in expectations between provider groups. Do all care partners know of the array of resource options available in a community, and if we do, do we all understand how to identify whether our patients’ needs align with the skill sets of these providers? It can be disastrous for our patients when they are transitioned to a level of support that does not align with their needs, whether lower or higher than is required for the patient. Either way, it leads to wasted resources and frustration for all involved.
David: There are mainly two problems with doing transition of care well. These are the interoperability of sharing information in disparate EHR systems and the other with providers who haven’t been well versed on how to facilitate the transition of care with other provider resources.
Todd: The transition of care as it relates to psychiatric treatment is often the most vulnerable and the most flawed. The shortage of mental health providers, coupled with the demand for services, creates strain on health systems that does not exist in any other area of healthcare. The lack of fair reimbursement and gaps in coverage create major barriers to successful transitions of care for those with severe or co-occurring psychiatric conditions. This is a systemic failure of U.S. healthcare policy and partially due to the fallacy of parity.
Bonnie: Poor transitions threaten patient safety, decrease consumer confidence in the healthcare system and waste resources. Poor coordination during transitions can result in confusion about the patient’s care, duplicative tests, medication errors, delays in diagnosis and lack of follow through on referrals.
Dr. Schultz: In the ideal situation, when a patient is referred or chooses to schedule as a new patient at our pain clinic, the first touch is typically a phone call during which an appointment is made by our telephone staff. Once the patient is registered in our system and the appointment made, medical records from the referring provider, or from previous relevant medical care, should move into our electronic medical record with minimal hassle and work for our business office staff. Unfortunately, this is not what happens.
By regulation, the patient must sign a Release of Information form, and this must be on file at the referring and/or sending medical practice before information from that practice can be sent to us. We can’t obtain a patient signature over the telephone, and this often complicates transfer of information.
Here are more frustrations we encounter with new patient referrals that could negatively impact patient care:
- Incomplete health records is the single biggest problem.
- Unrecognized medication conflicts because we do not have a complete medication list.
- Duplication of testing because we cannot determine what testing has been done.
- Difficulty reaching the referring provider after the consult to discuss the case.
- No referral received before we see the patient.
- Referral received, but it has incomplete information. It should include the reason for the consult with adequate detail, such as “Patient is being referred for back pain radiating to legs. Has been assessed and deemed not candidate for surgery. Please evaluate and treat pain using all appropriate means.”
- Recent clinic notes and relevant test and imaging results not included.
It is very often difficult to reach the referring provider to discuss the case. It would be helpful to have the referring provider’s cell phone number since calling clinic numbers means a wait on hold and often no contact with a provider.
How is your organization working toward solutions to these problems?
Dr. Schultz: We are assigning extra staff and creating additional workflows to make sure our providers have all the relevant medical information inside of our EMR before the patient encounter. This additional staff time is costly and requires a lot of manual work and rework.
On a more personal, peer-to-peer note, our providers try to reach the referring provider when possible right after the consult to discuss the case directly. Connecting with a busy referring provider in the middle of a busy clinic day is time-consuming and frustrating however for both our provider and the referring provider.
We try to contact the referring provider by phone for new patients but this is difficult and time-consuming. We generate a summary letter from our EMR that goes out to the referring provider. We call outside providers who are on the ROI for important information that cannot wait for mail.
David: As a pediatric orthopedic care provider who works with simple fractures to very complex patients, we not only recognize the importance of care transition but, fundamentally, have care coordinators in our operations who recognize the bidirectional aspects of what makes this work well. Part of the role of the care coordinator is to be aware of each step that can involve a transition of care and advocate for the patient as needed to insure that mistakes do not occur during transitions. It is through that intentionality that the system structure essentially drives the behaviors of our care team.
Lindsey: We believe that collaboration and organizational humility are essential. We focus on the strengths of our patients, their caregivers, our healthcare providers and our community-based organizations. We want patients to be connected to the most appropriate and person-centered resources. Our organization has developed local resource navigators that work with the clients to achieve this. The healthcare ecosystem in every community can be surprisingly larger than anyone would think, but also very complicated to navigate. We have no business making things more complex than we already have. Humility is something our industry struggles with, and we must make changes to ensure better outcomes for our patients.
Todd: PrairieCare has designed a continuum of psychiatric health services that allows patients to receive varying levels of care within the same system, often at the same location. We remained challenged by limitations with capacity and lack of viable funding for outpatient services. We continue to develop partnerships with other medical health systems and mental health providers alike to create more seamless transitions in care. We also supported the statewide psychiatric assistance line (PAL) that allows any healthcare provider free on-demand access to mental health triage and case consultation with a board certified psychiatrist.
Bonnie: Health Care Homes primary care clinics focus on improving care transitions with consistent and clear communication between all team members, including the patient. Communication should be patient-centered with regular followup communication by the care team and support from a care coordinator if needed. The primary care provider should be notified upon discharge from the hospital or other transitional care, and a followup appointment scheduled within 7-10 days post discharge. For patients discharged to home, we encourage in-home visits by a pharmacy student, community paramedic or community health worker to ensure a patient can follow their medication plan and safely manage at home.
What are some of the most common problems related to care transitions beyond your organization’s ability to address?
Lindsey: The overwhelming problem is funding and how funding for patient care is mapped. Resources provided to acute and clinical care delivery are critical; however, if much of the budget is directed to downstream care, there is minimal left for the support systems required to keep patients from returning into the care cycle. We must find ways to support the whole patient and connect with resources and services that can help them maintain optimal well-being. We need to consider the longevity of these services and prepare for a future where there will be an increased patient demand, especially among our rapidly growing older adult population. Working to direct funding to support our patients outside of the clinical environment is an important goal for us all.
Todd: The shortage of mental health providers and lack of local infrastructure results in access issues and barriers to needed placements. Much of this is due to inadequate funding and investment in services.
David: The most common problems we encounter are the ones that have happened upstream from the point when the patient comes under our care. These are mostly related patients whose previous providers have struggled with a lack of resources and continuity in the care they have provided. We see issues that have occurred because there has been poor planning around transitions and a failure to recognize that a patient’s health may involve much more than care from a single provider. We see patients who may come from a relatively great distance and sometimes end up with issues that could have been preventable or treated closer to home with a better awareness of the care transition process.
Bonnie: One of the biggest problems is seamless information exchange to alert appropriate care team members about a patient’s care transitions and the plan of care. Despite advances in technology, we do not communicate well across health systems and community services. Also, in some parts of the state, community services are simply not available for patients who lack family or friend support and need help with medication management, nutrition, transportation and other resources needed to stay healthy.
Confusion around medication is common. Medication instructions are not always clear, and patients have difficulty discerning between a generic and a brand name medication. If there is more than one provider involved in care, medication instructions can vary, making it difficult for the patient to follow directions.
Dr. Schultz: Some issues include important health status data that may not arrive at our practice in time for the patient encounter, including:
- When a patient comes to Nura from an oncologist, orthopedist or other specialty provider.
- When a patient goes from Nura to rehab or back to an oncologist.
- When a patient goes from Nura to an assisted living facility.
- Hospital discharge information. We may not have a complete history since information from the patient is often incomplete or inaccurate in detail.
Confusion around medication is common.
—Bonnie LaPlante
Are there legislative solutions to the problems around care transitions?
Todd: The state legislature has made the topic of mental health in our communities a priority and has invested deeply in start-up funding. However, the focus must be on parity and sustainability. Reimbursements for mental health services are on average 20% less than the rest of the medical community, and the authorization requirements are usually arduous. For example, an individual with diabetes can easily get access to a nutritionist covered by their insurance plan, yet someone with an eating disorder may have their benefits carved out by their plan, subject to different out of pocket rates, and will need to jump through additional hoops to get access to a nutritionist.
Bonnie: Legislative changes could improve the reimbursement model for primary care and care coordination by providing incentives for whole person care using an integrated patient-centered care team approach. Such provisions could provide financial support for taking time to work closely with patients to provide comprehensive coordinated care and to avoid negative health outcomes. Legislative action could also identify ways and funding to facilitate health information exchange and universal referral/care transition system software. Finally, there may be policy solutions to ensure a continuum of care and shared responsibility across organizations. For example, incentives could be put in place to encourage cross-setting integrated care teams to promote cooperation and accountability across health and community organizations.
Dr. Schultz: Improve HIPPA regulations so that medical care providers can exchange information more freely. Legislating improvement in the interoperability of medical records would also help. Better insurance transparency and better control of medication pricing could also be addressed at both a federal and state level in ways that better facilitate care transitions. Medications are a very important aspect of patient care, and patients often do not know what medications they are taking. The payers and pharmacies have this information, so having some accessible central database—similar to the PMP for opioids—that lists all active medications for each patient would be great. We would like to see better connectivity among the various EMRs to allow health information to flow more freely among different practices.
We would also like to see HIPAA rules adjusted as needed so HIPAA does not interfere with doctor to doctor communication about mutual patients.
Lindsey: TMedicare Advantage demonstrates through supplemental benefits that funding allotments for social determinants of health can impact the well-being of our older adults. CMS has allowed for plans to have flexibility in service options, and innovative advancements in this area should and will continue. On a state level, Medicaid could be encouraging more value-based reimbursement modeling. Adjustments to the funding model could encourage partnerships through the continuum of care and facilitate the breakdown of the current siloed methods. The current Medicaid waiver system is not sufficiently funded and creates sustainability concerns for providers throughout the state.
David:
There needs to be better understanding by government and industry around what needs to be done to address these issues. Things like portability acts and improving interoperability need clear pathways, which unfortunately have been very slow to emerge. The restrictions that we have in how we can practice across state lines can create unnecessary difficulties and limit the ability for a patient to seek the appropriate and needed care.
What are some examples of problems you see with care transitions between entities providing care before or after the patient comes to you?
Lindsey: We need standardized tools that help facilitate the transition of patients. Providers across the state can attest that we burden our teams and our patients with the many unnecessary and redundant steps systems our siloed approaches to care delivery have created. Patients can get lost, overwhelmed and often forego service opportunities due to our created barriers. We need better integration and mechanisms for aligning because we are exhausting everyone involved–including the patient.
Bonnie: One big problem is patients who do not understand their treatment plan, medications or the need for follow up appointments if they are feeling better. Patients with complex needs often require prompting or assistance to coordinate their care. Care transition is a vulnerable time for these patients.
Todd: Successful care transitions occur when providers are proactive in communication and clear in treatment planning. Another key undertone in care transitions in mental health is the presence of compassion–which is a palpable advantage. Problems exist when care providers fail to share necessary information, which may be complex factors such as historical trauma or social determinants of health. Not all care providers fully understand the breadth and diversity of psychiatric services, so that onus falls on our specialty to provide education on the continuum of care, including access protocols.
David: The biggest problem is communication, whether these are structured through systems that share the record or unstructured in the way care teams talk with each other to facilitate care.
Dr. Schultz: We see patients suffering more due to unnecessary rehospitalizations and inadequate care in assisted living facilities supporting chronic conditions.
Collaboration and organizational humility are essential.
—Lindsey Sand
What are some examples of positive systems that have been put in place by your organization or others to address care transition problems?
Dr. Schultz: An online patient-provider health information access portal accessible by patients and by providers is a great option that could be made easier and better to allow for seamless transfer of information.
Lindsey: We are fortunate to be piloting a program called Connected Communities, which allows our organization to facilitate efforts in care coordination, resource navigation and system simplification in our region. Together with community partners, healthcare providers, health plans and older adults, we have begun to implement impactful changes toward improved care transitions and the overall well-being of our community.
Todd: We have created patient experience groups and community forums to solicit feedback on care transitions and overall experience. Some of the feedback is tough and seemingly out of our control, but change starts with understanding. We continue to remain humble and optimistic about what we can do to best integrate psychiatric care and healing into the broader frame of healthcare.
Bonnie: Integrating a member of the primary care provider’s clinic team into the hospital discharge team and scheduling the followup appointment before discharge can be helpful. They can alert clinic staff to the reason for the visit and gather important medical information in preparation for the visit. They’ll have information to call the patient if they do not show up for an appointment or cancel the appointment.
Another positive example is the use of an ADT (admission, discharge, transfer) notification system to alert primary care providers to follow up with the patient based on established protocols.
David: One of the best examples we use and that we have seen colleagues use is the emerging role of care coordinators. These individuals may be employees of the clinic or hospital, contracted employees, and possibly even living in other states, by the clinic or hospital or employees of a third party payer such as an HMO or the state. They can be most effective with the highest level of healthcare training, such as an RN, and when they are actively going to the community and meeting with either patients or collaborative partners. They can assist in helping to proactively identify challenges around improving care transitions and how to overcome those barriers.
We would also like to see HIPAA rules adjusted.
—DR. David S. Schultz
How can better engagement of both the patient and their family improve the care transition process?
Lindsey: Providing the opportunity for patients and their families to have a voice is essential. Why would we design programming or a care plan for the patient without the patient at the center? That thinking has created the overly complicated ecosystem that we currently operate in. By creating a person-centered approach, we can aid the patient with their unique needs and address their barriers to optimal health. For instance, a discharging patient may receive orders for outpatient therapy; however, if that person lacks at-home support or is unaware of the transportation programming in their community, they will be unable to attend. Another example involves the swelling use of technology in healthcare. Technology has allowed us to deliver care in unique and essential ways, especially during the pandemic. However, if there are concerns with the digital literacy of the patient, have we taken the time to aid them through this?
Todd: In psychiatric healthcare, the patient experience and the patient outcome may not align, and in some cases, may even be divergent. Making progress towards treatment goals may require having difficult conversations with family members, facing fears and becoming vulnerable with care providers. This may create an uncomfortable experience but result in great outcomes. Conversely, mental health treatment that is focused solely on comfort and connections may produce a positive experience but limited outcomes. Our goal is to better engage with patients and families to align the experience and clinical outcomes and be assured that will continue through care transitions.
Bonnie: Patient and family engagement can improve health outcomes. Engaging patients and families through conversation, active listening, consideration of values and preferences and explaining healthcare choices can empower them to invest in their health. By choosing meaningful goals and developing a trusting relationship with their healthcare providers, patients and families are more likely to follow through and have improved outcomes.
David: The family and especially the patients themselves can play a critical role in helping assure that care transitions do not result in unnecessary complication. One way to engage them is through the improved and expanded use of portals that can help keep the patient and caregiver connected. Another engagement tool could employ aspects of the value-based reimbursement model that might even incent patients with lower premiums to take a more active role in their care.
What can physicians do to improve the process of care transitions?
Lindsey: Physicians are over-burdened, and they must lean more on the supports that exist for their patients outside the clinic or hospital. They may not be aware of the range of available support available to their patients, or they may not have the time or energy to flip through the hundreds of brochures that are dropped at their door. Regional collaboration among providers, community-based organizations and community members is required to relieve physicians and the entire care ecosystem transition barriers and improve care outcomes. We are all stretched extremely thin, and it is time that we begin to work more efficiently and in conjunction with one another.
David: They could have details about the care a patient has received before reaching them. This would include care by non-physician providers and they could have details about where the patient will receive care after they leave the physician. Being aware of the patient’s ability to understand and follow medical advice on their own, as well as understanding details about how that patient’s living conditions can impact outcomes, would be helpful. Many times, as much as a physician may want to do these things, there are systemic barriers. Things like incompatible EHR, privacy regulations, inadequate staffing and many others can work against optimal care transitions. Physicians must understand the patient as a whole and that it takes a village to provide whole patient care. We all must understand that it will take this same village to make the changes to the healthcare delivery system that will improve care transitions.
Bonnie: Physicians can champion, raise awareness and advocate for safe care transitions. They can support team members in having dedicated time to conduct tasks related to coordinating transitions, participate in quality improvement projects to determine how care transitions are working and implement strategies to improve and to measure progress. Primary care physicians can also build and maintain communication with hospital-based clinicians to facilitate care transitions.
Todd: When transitioning a patient’s care either to or from a psychiatric setting, it is critical that all providers are in alignment with care expectations and treatment goals. A focus on the whole person and not just the psychiatric condition will prevent marginalization of the person and their care. Cultural factors must also be considered, including any spiritual and religious aspects of treatment.
Dr. Schultz:
Being certain the patient understands what care they received so they can personally tell this to their other providers involved in care. If the patient goes to another provider, that provider should know about the care delivered at Nura. A lot is common sense, but sometimes having a formal process minimizes miscommunication.
Care transition should really have nothing to do with payment, but it often does.
—David J. Voller
How can tools and services like care coordination and medication management help address the problems posed by care transitions?
Todd: True interoperability is key to improving care transitions, yet it remains elusive for most providers. When health systems can ensure accurate and timely sharing of comprehensive and meaningful information, those coordinating care—even between organizations—and help to optimize the experience and outcomes for that patient. Especially in mental healthcare, where things like lab values and diagnostic imaging are not relevant, the importance of conveying the narrative of the care transition is amplified.
Bonnie: Care coordination’s main purpose is to organize care and share information with the patient and the care team to achieve safer and more effective care. Examples of care coordination approaches include teamwork, medication management and care management. Care coordination activities include communicating and sharing information, supporting patient’s goals and healthcare needs and establishing accountability and responsibility across a team, which helps to improve outcomes.
Patients with a care coordinator experience a one-on-one relationship that supports the patient and family in organizing patient care and navigating the healthcare system. The care coordinator helps the patient learn self-management skills, including medication management. The care coordinator also helps the patient recognize when medical intervention is necessary to maintain health and, if possible, avoid hospitalization.
Lindsey: Care coordination and management can make everything run more efficiently, provide better support for the client and empower the client to make the right decisions for their wellbeing. It breaks down barriers, drives compliance and can simplify care delivery. Effective medication management can address numerous challenges faced by our patients. At the time of care transitions, prescription additions or changes are common. Helping a patient through these changes is vital. As an in-home provider of many services, I can attest to the common occurrence of walking into a medication disaster. Examples are medication cabinets full of expired medications that were never wholly taken, discontinued medicines that the patient did not realize they were supposed to stop taking, and copies of medication records from past office visits or hospitalizations that are outdated but serve as a patient’s guide. We must recognize the challenges that some patients face with understanding medication adherence and aid them in addressing these.
What are some of the ways healthcare disparities create unique challenges related to care transitions?
Lindsey: This is the greatest obstacle. Despite exceptional clinical care, the patient will not be successful if we fail to recognize the personal disparities and determinants of health that patients experience in their homes, social lives and environment. We must marry clinical care with social care and advocacy for equity in our organizations, regions and across healthcare. This begins with raising awareness, improving cultural competency, ensuring access to necessary care resources (even if it may involve unique approaches, such as technology) and, once again, collaboration. We must elevate the standards in all state regions to ensure our entire population’s needs are addressed equitably.
David: Problems with healthcare disparities often originate with economic considerations, such as the ability to pay. Despite numerous assistance programs, some people may either distrust them, be unaware of them or simply unable to navigate them on their own. Even with navigation assistance they can be overwhelming. Care transition should really have nothing to do with payment, but it often does. There is no question access to care is impacted by affordability issues, which can have a distinctly limiting impact on how active a patient may be in the system of provider resources.
Todd: We know that patients are about 50% likely to follow through with referrals to mental health providers. When transitioning between care providers and different organizations, the referring provider or health system has an obligation to ensure that potential barriers such as transportation or insurance coverage are considered. In cases where health disparities exist, the importance of successful care transitions is magnified.
Bonnie: Patients who are vulnerable or at-risk often have poor access to care and may be underinsured or not insured at all. Lacking access to routine care, they may have untreated medical conditions, putting them at risk for chronic disease and acute health episodes. Other social factors, such as housing and employment stability, transportation and health literacy contribute to health disparities. All these factors need to be considered during care transitions when patients are most vulnerable.
Is there anything else about care transitions that you would like to discuss?
Lindsey: I’d like to reiterate the importance of elevating all health and community-based care providers’ significant roles in our communities. We are all part of the care safety net and play an essential role in patient well-being and health outcomes. Let’s strive for greater collaboration and recognition of one another and strive to break down silos and barriers to care.
Bonnie: Successful care transitions require intentionality and patient-centered care delivered by an integrated team to ensure that the patient remains safe and free of complications during a care transition. That means finding ways to fully understand each patient’s unique situation and designing care and support to help them be successful. It’s not something we can take on in silos. We have to work together. It’s the right thing to do to improve health outcomes.
David: At the end of the day it should have nothing to do with us but everything to do with the overall health of the patient/community. Care transitions involve developing partnerships along whatever continuum of care a given provider or provider group is involved in.The partnerships must have clear communication around expectations and capabilities. They must be adequately developed and reach far enough, realizing that not every patient will need every resource but, resources… for every possibility need to be in place. In the end, having these partnerships in care makes everyone’s job easier.
Todd: While the U.S. has one of the world’s most innovative healthcare systems, navigating its various components is overly-complicated and challenging. A patient suffering from acute or chronic health conditions should not have to shoulder the burden of care navigation. Those suffering from psychiatric illnesses are often carrying additional stressors, which impact one’s ability to manage care transitions and follow through on medical advice. The costs associated with untreated psychiatric illness and improperly treated co-occurring conditions is extraordinary, and effective care transition is a critical step, maybe the most critical, in ensuring positive experience and outcomes. Health system and insurance companies must accept this responsibility and prioritize helping patients manage transitions successfully as a core part of the care itself.
I’ve often talked about the gap where the money isn’t. Providing treatment for diagnosed psychiatric conditions within our clinics and hospitals are covered. However, many patients require additional support to navigate care that has no way of being funded. Care navigation services and case management are accessed differently by payer source or county of residence. Access can be confusing or arduous, meaning many don’t receive this support at all. Many outpatient services are poorly reimbursed, and intensive services like psychiatric residential treatment facilities (PRTFs) are not even covered by most commercial insurance in Minnesota. As long as these gaps exist, the onus and the honor of care transition will remain with providers.
the panelists
Todd Archbold, LSW, MBA after joining PrairieCare in 2006 Todd became chief executive officer in 2020. He has helped develop one of the region’s largest psychiatric health systems with 12 locations in Minnesota. He is also the executive director for the Psychiatric Assistance Line (PAL) – a statewide service aimed towards increasing collaboration and support between psychiatry and primary care.
Bonnie LaPlante, MHA, BS, RN is the health care home (HCH) program director, in the Health Policy Division, at the Minnesota Department of Health, where she has worked for over nine years. She has 16 years of leadership experience as a clinic services nursing director, as well as experience as a director of a home health agency and a coordinator in long term care..
Lindsey Sand, LHSE, NHA serves as vice president of population health for Knute Nelson, an aging services organization offering a full continuum of services across more than 35 counties in northwestern and central Minnesota and eastern North Dakota. She serves on the boards of Lakes Area Age-Friendly, LeadingAge Minnesota and the LeadingAge Minnesota Foundation.
David S. Schultz, MD, MHA is the medical director and founder of Nura Pain Clinic. Dr. Schultz is a board certified anesthesiologist with additional board certification in pain medicine from the American Board of Anesthesiology, the American Board of Interventional Pain Physicians and the American Board of Pain Medicine. He has been a full time interventional pain specialist since 1995.
David J. Voller, MBA, FACHE is the clinic administrator at Shriners Children’s Twin Cities. His 30-year career in health care includes positions at the Mayo Clinic, Gillette Children’s and BWBR. David is a Fellow of the American College of Healthcare Executives, sits on the board of ACHE MN and chair for membership and advancement.
About the sponsors
Coverys is a medical liability insurance company that combines insurance protection with risk analytic services. They are a national leader in the field with over 45 years experience protecting health care.

LeadingAge Minnesota Foundation supports initiatives to transform and enhance the experience of aging by building the workforce for tomorrow, advancing promising new approaches to service delivery and developing leadership at all levels.

Nura Pain Clinic was created by physicians who are pioneers in precision pain management. For over three decades they have specialized in therapies and procedures helping those who struggle with chronic pain get their life back.

RAYUS Radiology, formerly CDI, is a nationwide leader in advanced diagnostic and interventional radiology. Blending the art and science of well-being, RAYUS is revolutionizing radiology and making the unknown known for over a million patients and their providers each year.
MORE STORIES IN THIS ISSUE
cover story one
Co-opetition: An emerging trend in health care
By David J. Voller, MBA, FACHE
cover story two
COVID-19 Litigation: Cases and Defenses
BY Sandra M. Cianflone, J.D.
capsules
Top news, physician appointments and recognitions
Interview
Moving Medical Education Beyond the Classroom
Meghan Walsh, MD MPH FACP
Senior Care
Connected Communities: Aging well in greater Minnesota
BY MARK ANDERSON, MBA, CEO
Minnesota health care roundtable
Care Transitions: Improving the safety net
Patient Perspective
The Impact of COVID on People with Disabilities: A need for proactive planning
By Joan Wilshire, MPA
AUGUST 2024
cover story
Assessing and Advancing Community Health: The overarching value of equity
BY Brooke Cunningham, MD, PhD
CONTACT
(612) 728-8600 | comments@mppub.com
758 Riverview Ave | St. Paul MN 55107
© Minnesota Physician Publishing · All Rights Reserved. 2023
quick links
We welcome the submission of manuscripts and letters for possible publication. All views and opinions expressed by authors of published articles are solely those of the authors and do not necessarily express those of Minnesota Physician Publishing Inc., or this publication. The contents herein are believed to be accurate but are not intended to replace medical, legal, tax, business or other professional advice or counsel. No part of this publication may be reprinted or reproduced without written permission from our publisher.