may 2022
VOLUME XXXVI, NUMBER 01
May 2022, VOLUME XXXVI, NUMBER 02
Capsules
Mayo Announces $49 Million Rochester Laboratory Expansion
The Mayo Clinic has recently announced that it is investing in a $49 million laboratory expansion project in Rochester. Construction for the project has started and will continue through 2025. The expansion will increase laboratory space at Mayo Clinic’s Superior Drive Support Center. The new space will house several clinical laboratories that reside in the Hilton Building, which is part of Mayo Clinic in downtown Rochester. Relocation of these laboratories to Superior Drive Support Center will allow them to expand and take advantage of more modern facilities. The expansion will include a new laboratory space for five clinical testing labs, new laboratory space for Mayo Clinic Biopharma Diagnostics and new laboratory support staff spaces at Superior Drive Support Center. The expansion project also will help achieve Mayo Clinic Laboratories’ strategy to provide diagnostics to Mayo Clinic patients across the U.S. and abroad. Patients will have access to laboratory testing through their health care team at Mayo Clinic, while health care teams around the world will have access to testing through Mayo Clinic Laboratories’ Test Catalog. In addition to the available tests, Mayo Clinic’s Department of Laboratory Medicine and Pathology is continuously innovating to introduce new tests as health care and diagnostics advance. “Laboratory diagnostics and interpretations are front and center when it comes to the patient journey,” says William Morice II, M.D., Ph.D., president of Mayo Clinic Laboratories. “The COVID-19 pandemic shined a light on the importance diagnostic testing plays within the overall health care system, and we are committed to expanding our testing to meet the needs of patients we serve at Mayo Clinic and through Mayo Clinic Laboratories.” Dr. Morice chairs Mayo Clinic’s Department of Laboratory Medicine and Pathology.
HealthPartners Reports Large Income Increase
At their annual online meeting held the third week of April, HealthPartners reported record claims for health care services in 2021, as well as a $150 million increase in operating income. Unexpectedly high use of health care services lead to the increase, up by over 50% from 2020. Beyond COVID treatments, patients who had delayed seeking medical attention during the pandemic returned in record numbers for routine care and services. Andrea Walsh, HealthPartners chief executive, said “In 2021, we saw our highest-ever claims costs, paying more than $3.6 billion for members’ care. We saw more patients in the hospital who were sicker and needed to stay in the hospital longer. We saw people who had held back from getting care and then came into our clinics and hospitals needing care for illness and injuries well beyond COVID.” In 2021, HealthPartners paid $7.6 billion in expenses from revenue of $7.75 billion, leaving operating income of more than $150 million — a 56% increase over operating income of $96 million in 2020. It was the second year of improved results following an operating loss in 2019. Last year’s operating profit margin was about 2%, meaning HealthPartners saw 2 cents of operating income for every dollar of revenue. “When we came into 2021, we had pent-up demand that came through the system, resulting in higher claims cost in 2021, but offset by higher volumes on the care side of the organization,” said CFO Penny Cermak. They also reported providing more than 900,000 system-wide telehealth visits during 2021, many related to behavioral health. Walsh cited that over the course of the last two years and moving into the third year of the pandemic, the demand for mental health and the need for mental health services continues to increase.
Minnesota’s Uninsured Rate at Historic Low
New data released by the Minnesota Department of Health shows actions taken by state officials and the Biden administration helped drop the state’s uninsured rate in 2021 to 4.0%, the lowest level ever measured. “The Minnesota Heath Access Survey shows that more Minnesota families have been able to access and maintain their health insurance during this critical time,” said MNsure CEO Nate Clark. “Minnesota has been able to reduce the uninsured rate thanks in part to targeted, effective policies, including the expansion of premium tax credits that lower the cost of monthly premiums for private health plans available through MNsure.” The 2021 federal American Rescue Plan (ARP) relief package expanded access to subsidies to those who were ineligible previously and lowered costs for tens of thousands of Minnesotans who purchase health insurance through MNsure, the state’s health insurance marketplace. The cost savings drove a record number of sign-ups for MNsure as over 134,000 Minnesotans enrolled in 2022 health coverage – a 10% increase from last year. The enhanced benefits made available through the ARP are set to expire at the end of 2022 unless the U.S. Congress acts to extend them. “To keep Minnesota’s uninsured rate at this historic low and to help address the racial disparities in health coverage in our state, Congress must act to extend these cost-saving benefits,” said Clark. “Failure to act could increase out-of-pocket costs for thousands of Minnesotans and push some to drop their coverage entirely.” MNsure estimates that without congressional action to extend the benefits, about 70,000 Minnesotans who currently access premium tax credits through the marketplace will see higher out-of-pocket costs when the new plan year starts in January 2023. Over 10,500 individuals are estimated to lose access to all of their current financial help. Without an extension, MNsure estimates that net premium spending across the state may increase by 30% to 40%, or an average of $1,314 per year for those receiving premium tax credits. Some regions could see even bigger increases.
U of MN Researchers Develop Smart phone “lab-in-a-chip”
A University of Minnesota research team has developed a new microfluidic chip for diagnosing diseases that can be powered wirelessly by a smart phone. The innovation opens the door for faster and more affordable at-home medical testing. Microfluidics involves the study and manipulation of liquids at a very small scale. One of the most popular applications in the field is developing “lab-on-a-chip” technology, or the ability to create devices that can diagnose diseases from a very small biological sample, blood or urine, for example. The research is published in Nature Communications, a peer-reviewed, open access scientific journal published by Nature Research. Scientists already have portable devices for diagnosing some conditions — rapid COVID-19 antigen tests, for one. However, a big roadblock to engineering more sophisticated diagnostic chips is the fact that they need so many moving parts. The University of Minnesota team was able to create a microfluidic device that functions without all of those bulky components. “It’s not an exaggeration that a state-of-the-art, microfluidic lab-on-a-chip system is very labor intensive to put together,” said Sang-Hyun Oh, an electrical and computer engineering professor and senior author of the study. “Our thought was, can we just
get rid of the cover material, wires and pumps altogether and make it simple?” The breakthrough involves the same technology used for contactless smart phone payment in stores. “This is a very exciting, new concept,” said Christopher Ertsgaard, lead author of the study. “During this pandemic, I think everyone has realized the importance of at-home, rapid point-of-care diagnostics. And there are technologies available, but we need faster and more sensitive techniques.” Oh’s lab is working with Minnesota startup company GRIP Molecular Technologies, which manufactures at-home diagnostic devices, to commercialize the microchip platform. The chip is designed to have broad applications for detecting viruses, pathogens, bacteria and other biomarkers in liquid samples. “To be commercially successful, in-home diagnostics must be low-cost and easy-to-use,” said Bruce Batten, founder and president of GRIP Molecular Technologies. “Low voltage fluid movement, such as what Professor Oh’s team has achieved, enables us to meet both of those requirements.”
New Program Addresses PCS Shortage Crisis
The Metropolitan Center for Independent Living (MCIL), in part through a $208,000 Community Innovation Grant from the Bush Foundation, has recently announced its plans to develop a first-ever credit-based curriculum leading to the credential of a Certified Personal Care Assistant. Facing an unprecedented national crisis in hiring and retaining direct care workers, also referred to as Personal Care Assistants (PCAs), the new program will give individuals access to a career offering professional growth opportunities, living wages, and immense personal rewards. There are nearly 140,000 people employed in the direct care workforce in Minnesota. Among those that require services from this workforce are 612,000 Minnesotans with a serious disability. Our elderly population, another demographic that relies on PCAs, was 865,000 in 2018 and is projected to rise to 1,262,000 by 2030. The direct care workforce has the highest percentages of female and diverse workers of any workforce sector and will see increased demand for services in the coming years. The Certified Personal Care Assistant program addresses the workforce shortage while advancing economic equity through an industry-adopted credentialed career. “I do not know of a more severe crisis than what we are experiencing today in the home and community base services system with so many closings of group homes, nursing homes, severe worker shortages throughout our Long-Term Services and Supports system including Minnesota’s PCA Programs” said Jesse Bethke Gomez, MCIL Executive Director. As part of a three-year study that involved many stakeholder groups, MCIL played a critical role in drafting the report “Recommendations to Expand, Diversify and Improve Minnesota’s Direct Care and Support Workforce.” In response to the report and in recognition of the workforce crisis, in 2021 our state legislature passed into law the Minnesota PCA Rate Framework, which considers competitive workforce factors such as compensation. The new law, together with the Certified Personal Care Assistant program, will help solve problems that have daunted the PCA workforce and lead to higher, livable wages.
Fulcrum Health, Inc. announces 2022 ChiroCare Centers of Excellence
Fulcrum Health, Inc., a nonprofit physical medicine management organization committed to leveraging chiropractic care to transform healthcare, recently announced the 2022 list of ChiroCare Centers of Excellence. The designation recognizes the ability to meet evidence-based guidelines and stringent quality standards designed to put patients at the center of the treatment experience. The ChiroCare Centers of Excellence designation grew out of Fulcrum Health’s 2013 National Task Force on Spine Care, which identified the key qualities of clinics that exemplify a value-based, patient-centered approach to advancing the treatment of low back pain. This year’s additions bring the number of ChiroCare Centers of Excellence to a total of 193 providers at 102 locations across Minnesota, Wisconsin and South Dakota. “Providing health care needs and meeting patient expectations has changed dramatically in recent years, and the patient experience has become more complex. Providers who put patients at the center of the care experience can improve clinical outcomes while helping patients feel supported and engaged in the process,” said Dr. Vivi- Ann Fischer, Chief Clinical Officer, Fulcrum Health. “Our ChiroCare network consists of more than 2,900 providers who deliver outstanding care to over 2 million patients. The Centers of Excellence designation celebrates those clinics that go above and beyond to put patient-centered standards of quality at the core of their operations.” Fulcrum Health identifies ChiroCare Centers of Excellence through an application and document review process. To earn recognition, clinics must meet criteria related to shared decision-making between provider and patient to create goals of care, motivational interviewing and biopsychosocial assessment, documentation of measurable goals and conservative use of radiology. Also considered are exercise instruction to empower patient self-care, home care and prevention education and patient care coordination Fulcrum Health recognized the first ChiroCare Centers of Excellence in 2016”
Cuyuna RegionalHospice ProgramNamed Honors Recipient
Cuyuna Regional Medical Center was recognized earlier this month for providing the highest level of quality, as measured from the caregiver’s point of view, by being named a 2022 Hospice Honors recipient. The award was bestowed by HEALTHCAREfirst, a leading provider of billing and coding services and utilized Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey data. “Hospice Honors recipients are industry leaders in providing quality care and constantly seeking ways to improve,” said Ronda Howard, Vice President Revenue Cycle at HEALTHCAREfirst. “We are honored to be aligned with such high performing agencies like CRMC and we congratulate them on their success.” Award recipients were identified by evaluating performance on a set of 24 quality indicator measures. Performance scores were aggregated from all competed surveys and were compared on a question-by-question basis to a National Performance Score calculated from all hospices contained in the HEALTHCAREfirst’s Hospice database. CRMC’s Director of Home Care/Hospice Jennifer Wiedell credits the entire team’s efforts to provide exceptional, respectful, personalized care for being named a 2022 Hospice Honors recipient. “This award shines a light on the hard work of our entire team including physicians, nurses, aides, social workers, therapists, the chaplain, massage therapist, administrative team and volunteers,” Wiedell said. “All patients and families deserve high-quality medical care at the end of life, which is why we remain focused on supporting them in living each day to the fullest. Our team takes pride in providing the best possible patient experience, and we are honored to receive this award.”
MORE STORIES IN THIS ISSUE
cover story one
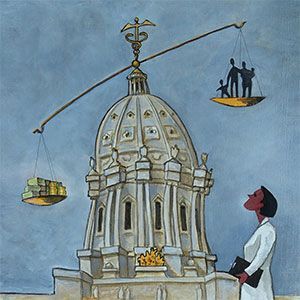
Co-opetition: An emerging trend in health care
By David J. Voller, MBA, FACHE
cover story two
COVID-19 Litigation: Cases and Defenses
BY Sandra M. Cianflone, J.D.
capsules
Top news, physician appointments and recognitions
Interview
Moving Medical Education Beyond the Classroom
Meghan Walsh, MD MPH FACP
Senior Care
Connected Communities: Aging well in greater Minnesota
BY MARK ANDERSON, MBA, CEO
Minnesota health care roundtable
Care Transitions: Improving the safety net
Patient Perspective
The Impact of COVID on People with Disabilities: A need for proactive planning
By Joan Wilshire, MPA
AUGUST 2024
cover story
Assessing and Advancing Community Health: The overarching value of equity
BY Brooke Cunningham, MD, PhD
CONTACT
(612) 728-8600 | comments@mppub.com
758 Riverview Ave | St. Paul MN 55107
© Minnesota Physician Publishing · All Rights Reserved. 2023
quick links
We welcome the submission of manuscripts and letters for possible publication. All views and opinions expressed by authors of published articles are solely those of the authors and do not necessarily express those of Minnesota Physician Publishing Inc., or this publication. The contents herein are believed to be accurate but are not intended to replace medical, legal, tax, business or other professional advice or counsel. No part of this publication may be reprinted or reproduced without written permission from our publisher.