May 2022
VOLUME XXXVI, NUMBER 02
May 2022, VOLUME XXXVI, NUMBER 02
Interview
Moving Medical Education Beyond the Classroom
Meghan Walsh, MD MPH FACP
Besides your work as a hospitalist, you are the chief academic officer at Hennepin Healthcare. Please tell us about what that work entails.
Hennepin Healthcare is a teaching hospital and clinic system. We have over 300 residents and fellows physicians who train in over 30 specialties here. We also have nearly 100 medical students who come to Hennepin for their clinical training. Once you are a practicing physician, you are also expected to continue to advance your knowledge in your specialty. My job is to ensure this clinical learning environment is the best it can be for all of these learners, from a college student interested in medicine to a first year medical student to a seasoned faculty physician who has been in practice for 40 years. I also play a role in strategy for the organization—ensuring we are a dynamic learning organization now and well into the future. I have the best job!
As a teaching hospital, how has the importance of what HCMC provides increased with the changing ways physicians are fulfilling CME requirements?
Medical education has been a key part of our mission for over 100 years. So much has changed and evolved in how we teach and how we learn during this time. Advancing technology, competency-based medical education change and the practice of medicine in this complex environment has led to new knowledge gaps and needs and opened the door to novel ways to close those gaps. We have moved beyond the classroom and traditional teaching methodology. Technology has allowed us to create more engaging coursework that is more flexible and comprehensive. This was critical during the peak of COVID -19, as it allowed us to continue to safely teach and learn in new ways. We have also developed incredible simulation-based training that allows us to hone our skills in high acute settings, improve teamwork training and continuously improve our competency with rare but essential procedural skills. Our future will require more partnerships with communities in Greater Minnesota to share expertise and advance our collective knowledge and practice.
The Hennepin Healthcare Research Institute (HHRI) has been active since 1951 improving health care and is recognized as a national leader. What are some of the projects they are working on now?
HHRI plays a critical research role in Minnesota. Many are surprised that we consistently rank in the top 10% nationally of institutions receiving National Institutes of Health (NIH) grant funding. Our four focus areas of research align with our expertise as a health care safety net: addiction medicine, trauma, infectious disease and health services research.
Our unique role as teachers, researchers and clinicians, as well as our commitment to equity and inclusion, placed us at the leading edge of research and care during the pandemic. If you were a patient coming to Hennepin in the early stages of the pandemic, you had the opportunity to participate in Remdesivir trials (COVID antiviral therapy,) convalescent plasma immune therapy trials, COVID-19 PCR testing with rapid result turnaround, life support and intensive care for the sickest of our patients. As one of the first labs to build testing protocols, we quickly became the testing resource for the state and other health systems in town. But our mission led us to the focus on the disparities arising from this pandemic. We brought testing to skilled nursing facilities and jails to quickly test and isolate affected patients in these high risk settings. When we deploy research alongside great clinical care and train others to these evolving systems, we quickly iterate our care to meet any clinical challenge; navigating the COVID-19 pandemic was no exception.
More recently, we have nurtured greater partnerships with our community and plan to attend Open Street Festivals to co-create solutions to the health care challenges facing Minnesotans. The future of research is ending the disparities that exist in health care today.
Our community partnerships are critical to our mission.
While HCMC is perceived as a safety net hospital, there are several other hospitals with a much higher percentage of Medicare reimbursement. What are some of the misconceptions about your patient mix?
I don’t think people understand the truly unique role Hennepin Healthcare holds in the Minnesota health care landscape. While there are other hospitals that take care of more patients covered by Medicare, HCMC stands alone in the percentage of revenue that comes through Medicaid (health care paid by a state and federal partnership for people who meet certain requirements around income, disability and family status). In data provided to us by the Minnesota Department of Human Services, adult patients covered by Medicaid getting primary care from our system have significantly higher rates of chronic conditions than other Minnesota adults on Medicaid. In that same data set, we see our adult patients have experienced homelessness at more than double the rate of other Medicaid-covered adults. Lastly, the majority of our patients identify as BIPOC, reflecting the dynamic diversity of the communities we serve.
What are some of the other things people may not understand about HCMC?
Most people know that we are an adult and pediatrics Level 1 Trauma Center, but we are way more than that. We have a downtown hospital and eight primary care and specialty clinics throughout the metro area. We have a cutting-edge Hyperbaric Chamber which supports the region; last year we had over 5,500 treatments. We also have an integrated emergency care set of services, including our Emergency Department which had over 93,000 visits last year and 87,000 ambulance runs. The Midwest Poison Control Center resides here. Our mental health care is some of the best in the state and includes inpatient care, outpatient care and the Redleaf mother baby center. Our community connection care ring includes hospice care and Minnesota Visiting Nurses Association home care, as well as the jail and healthcare for the homeless services.
When our state faces an emergent health risk, we are there. We have experts in Emergency Preparedness who have led us through the I-35W bridge collapse and the COVID-19 pandemic.
In every session, the State Legislature considers bills that impact how healthcare is delivered. What are some of potential improvements you would like to see enacted?
The flexibilities in health care regulations during the public health emergency (PHE) provided a time to test some innovations in health care we otherwise would not have been able to trial, and we made some incredible strides forward because of them.
During the PHE, patients on Medicaid were able to stay enrolled without additional paperwork for a full year, instead of jumping through the hoops of reenrollment multiple times per year as we did pre-PHE. Previously, many people would churn off and on the program throughout the year, causing significant costs to the state, insurance companies and providers, as well as major disruptions to patient care when people suddenly found themselves without insurance coverage because they had moved and missed a letter, or missed a deadline or their income varied one month to the next. Throughout the PHE, the federal government allowed continuous eligibility for anyone on Medicaid, verifying eligibility only once per year. Verifying eligibility one time per year was be a game changer for consistency in care and lowering costs to our system for unnecessary bureaucratic and administrative burdens.
Allowing easier access to telehealth during the PHE has changed how we provide care, as we were opening up clinical connections frequently missed before. These flexibilities in telehealth must continue for patient access–we could take their lunch hour to meet with a doctor instead of taking a half day of vacation, they could forego a three hour drive from Greater Minnesota and instead spend 30 minutes on video with a specialist. The access to video for appointments was apparent, but we must not let access to audio be considered a second rate service. Video is ideal, but in those situations where it is not possible, we need to ensure audio continues to be reimbursed at a rate that incentivizes the option to keep it available to patients.
What changes in how you can provide care have the recent extensive expansion of the hospital made for your patients?
Several years ago, we built our beautiful Clinic and Specialty Center (CSC) in downtown Minneapolis. It has allowed to us centralize our primary care and subspeciality clinics into one downtown setting. In addition to the primary care clinics located throughout the metro, has helped us provide better access to residents of Hennepin County. The CSC incorporates many local artists’ work and has an abundance of natural light; it feels like a healing environment right when you enter. The onsite parking, new operating rooms and bigger clinic spaces allow for a better experience for our patients.
The pandemic has stretched the concept of physician burnout well beyond what was already a significant issue. What are some of the ways you are addressing these concerns?
Physician burnout is definitely impacting our physicians, our residents and even our medical students like never before. Research has shown that psychological wellbeing connects to several pillars including autonomy, competence and relatedness. Medicine is no different. Medicine has pushed productivity—the movement to see more patients in less time. This has made patient care more of a transaction than a connection. The pandemic added new challenges: exhausting work, the lack of a playbook and available treatments, coupled with a feeling of powerlessness both in treating patients with infection and watching others unable to access their primary care, necessary procedures and critical addiction and mental health support. Our mitigating interventions have centered around building back autonomy in clinical schedules and work, offering easy access to mental health services and fostering onsite connectedness and belonging.
HCMC has many unique partnerships with both large and small organizations providing health care. What can you tell us about some of these and what future partnerships may be in store?
Our community partnerships are critical to our mission, our success and ability to transform healthcare in ways that benefit our patients well into the future. One of the exciting directions I see is related to our commitment to diversity and inclusion at Hennepin. Our Chief Equity Officer, Dr. Nneka Sederstrom, has helped to build a pathway that introduces high school students of color to health care professions and professionals at Hennepin. We are also building business relationships with minority businesses in the community. We all do better when working together.
Meghan Walsh, MD MPH FACP
is the chief academic officer at Hennepin Healthcare, the associate dean for affiliate hospitals, and an associate professor of internal medicine at the University of Minnesota School of Medicine. She has worked as a hospitalist for over 15 years.
MORE STORIES IN THIS ISSUE
cover story one
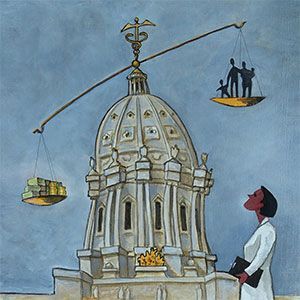
Co-opetition: An emerging trend in health care
By David J. Voller, MBA, FACHE
cover story two
COVID-19 Litigation: Cases and Defenses
BY Sandra M. Cianflone, J.D.
capsules
Top news, physician appointments and recognitions
Interview
Moving Medical Education Beyond the Classroom
Meghan Walsh, MD MPH FACP
Senior Care
Connected Communities: Aging well in greater Minnesota
BY MARK ANDERSON, MBA, CEO
Minnesota health care roundtable
Care Transitions: Improving the safety net
Patient Perspective
The Impact of COVID on People with Disabilities: A need for proactive planning
By Joan Wilshire, MPA
AUGUST 2024
cover story
Assessing and Advancing Community Health: The overarching value of equity
BY Brooke Cunningham, MD, PhD
CONTACT
(612) 728-8600 | comments@mppub.com
758 Riverview Ave | St. Paul MN 55107
© Minnesota Physician Publishing · All Rights Reserved. 2023
quick links
We welcome the submission of manuscripts and letters for possible publication. All views and opinions expressed by authors of published articles are solely those of the authors and do not necessarily express those of Minnesota Physician Publishing Inc., or this publication. The contents herein are believed to be accurate but are not intended to replace medical, legal, tax, business or other professional advice or counsel. No part of this publication may be reprinted or reproduced without written permission from our publisher.