July 2024
VOLUME XXXVIII, NUMBER 4
AUGUST 2024, VOLUME XXXVIII, NUMBER 5
Capsules
HealthPartners to Leave UnitedHealthcare Medicare Advantage Network
Citing rates of claims denial up to 10 times higher than that of other insurers it works with, HealthPartners recently announced it would be leaving the UnitedHealthcare (UHC) Medicare Advantage Network starting next year. In a public statement the health plan said, “UHC delays and denies approval of payment for our patients’ Medicare Advantage claims at a rate unlike any other insurer in our market. Unfortunately, some of UHC’s practices create unnecessary waits and delays for patients, and they interfere with our ability to provide patients with timely and appropriate care.” It is unusual to leave a health plan network but the decision came after a year of negotiations. The change applies to care provided at HealthPartners and Park Nicollet clinics and hospitals, including Methodist, Regions and Lakeview hospitals. HealthPartners will be offering additional resources and information to help those affected by the change, which can be found online. In reaction to the announcement, UHC said, “We proposed a contract that provided solutions HealthPartners sought to continue participating in our Medicare Advantage network. Rather than using the remaining time on our contract to implement these solutions, HealthPartners rescinded its position and is now putting Medicare Advantage patients in the middle of our negotiation, unnecessarily creating stress and fear for them while spreading outlandish, false claims. Our goal is to utilize the remaining months on our contract to reach an agreement that ensures the people we serve have continued network access to HealthPartners. We hope HealthPartners shares our commitment to provide access to care for all Minnesota and Wisconsin residents.” For now, UHC’s Medical Advantage members will continue to have network access to HealthPartners facilities and physicians through the end of the year and UHC will continue to work toward a compromise. Last week, 11 people were arrested outside the UHC headquarters in Minnetonka for protesting what they alleged is the company’s practice of not paying for care. An organizer for the protest said that UHC leadership has “refused to acknowledge that prior authorizations and claim denials are a widespread problem.”
Rainbow Health Announces Closure
Rainbow Health, a longstanding provider of support services to Minnesota’s LGBTQ+ community, individuals living with HIV and those facing barriers to equitable healthcare, recently announced that it had reached a point where continuing operations was no longer sustainable. The closure was effective immediately, unexpectedly affecting both clients and employees. A statement posted on its website said, “We are actively working with local organizations to continue providing the critical services that our clients depend on. Clients will be informed of alternative care options, and we will facilitate the secure transfer of medical records in accordance with HIPAA guidelines.” Less than two weeks after the announcement the Minnesota Department of Human Services (DHS) announced it had reached an agreement with the Aliveness Project to expand its service delivery as an HIV supports provider. The Aliveness Project supports people living with, and at the greatest risk of HIV, through transformative resources and direct services. For the past 40 years it has pursued the single mission of empowering healthy, self-directed lives. The loss of Rainbow Health left thousands of Minnesotans living with HIV without access to emergency assistance such as rent checks, utility support, food access and insurance navigation. “HIV support services are so important to the people who rely on them,” said Human Services Commissioner Jodi Harpstead. “We’re grateful the Aliveness Project is willing and able to take on this critical work. We’re also thankful to our partners who worked with us to meet client needs while finding this solution.” Under the new agreement, the former Rainbow Health contract responsibilities will be transferred to the Aliveness Project, effective immediately, while it works with partners to coordinate the details of the transition. Keeping people in stable housing and limiting any interruption of other basic life needs continues to be the priority of the state response. As Aliveness works to re-establish services, questions about immediate needs can continue to be directed to the Ryan White Programs Customer Care Line at DHS: 651-431-2398.
MAFP Releases Long COVID Webinars
To The Minnesota Academy of Family Physicians (MAFP) recently released a series of webinars to assist physicians with recognizing and managing long COVID. Research has shown that many providers do not feel equipped to recognize, diagnose or manage long COVID. To help combat this, MAFP partnered with Stratis Health and the Minnesota Department of Health (MDH) Long COVID Guiding Council to produce three webinars, each about an hour long and now available on demand. Long COVID and post-COVID conditions are health problems that people experience after having COVID and that are present for at least three months as a continuous, relapsing and remitting, or progressive disease state affecting one or more organ systems. Sometimes the long-term symptoms are severe enough to interfere with daily life activities, work, school, caregiving, exercise and other activities that help people thrive. A subset of people will have very severe symptoms that leave them newly disabled. The series covers the following:
Session 1: Recognizing long COVID. Includes differentiating long COVID from other chronic conditions with similar presentations; identifying different long COVID symptom patterns; understanding the potential stigma and other psychosocial concerns that patients with long COVID may experience; and gaining awareness of resources available to people experiencing long COVID.
Session 2: Long COVID in pediatric and geriatric populations. Includes understanding the role of long COVID in the context of other conditions affecting older adults and an overview of available tools and resources to support older adults; differentiating long COVID from other chronic conditions in pediatric populations and an overview of available tools and resources to support families.
Session 3: Treatment and management options for long COVID and equity considerations. Includes establishing familiarity with current treatment and management options for long COVID; understanding when to seek specialty referrals; and considering how equity may play a role in patients’ ability to seek care.
The Long COVID ECHO Series for Health Care Providers is available on YouTube at https://www.youtube.com/playlist?list=PLrX6m5cvp8hCbPkungsFtgh_7y-ywIBC7.
Please note that there are no CME credits for watching the recordings. More provider education resources, including free CME credits, are linked on the MDH website: For Health Care Providers: Post-COVID Conditions - MN Dept. of Health (state.mn.us).
UnitedHealthCare Sues State of Minnesota
UnitedHealthCare (UHC) recently filed suit over new policies included in the recent omnibus bill that prohibit for-profit HMOs from operating Medicaid health plans. The lawsuit names Minnesota Attorney General Keith Ellison, Minnesota Department of Human Services (DHS) Commissioner Jodi Harpstead and the State of Minnesota as defendants. The company wants provisions that apply to HMOs in the state Medicaid program stricken from the law. “UnitedHealthcare is challenging legislation that limits choice for individuals, families and children in Minnesota,” UHC said in a statement. “Minnesotans deserve the right to choose among health plans that offer the broadest access to care, the most innovative services and the highest quality benefits to meet their health care needs.” UHC argues that the omnibus bill passed in May violates the “single subject clause” in the Minnesota constitution, which states, “No law shall embrace more than one subject, which shall be expressed in its title.” The suit states that both the provision and the omnibus bill itself are unconstitutional. Since 2022, UHC has managed two Medicaid programs for Minnesotans enrolled in Families and Children Medical Assistance, and MinnesotaCare. Only around 32,000 individuals have coverage through UHC through a contract awarded by DHS only two years ago. While UHC claims it has a 1% profit margin on this coverage it apparently justifies what could be a complex legal challenge. UHC claims that informing their customers of the need to select a new plan “will cause irreparable harm to its business and goodwill, as well as to its members who chose its plans and will be forced off them.” Considering that parent company UnitedHealth Group saw its revenues grow to $371.6 billion in 2023, a $47.5 billion or 14.6% increase from the previous year and that operational earnings were up $32.4 billion or 13.8% in that year, these arguments are puzzling. Nonetheless, UHC wants the provisions stricken from the new law that prohibit them from collecting money generated by Minnesota taxpayers to administer health care benefits to individuals covered by state safety net programs.
Safe Harbor Program Reports Positive Growth
A recent evaluation report from the Minnesota Department of Health (MDH) showed its Safe Harbor program served more youth from 2021 to 2023 than in previous years and found high levels of program satisfaction. The Safe Harbor program is a multi-agency, statewide initiative designed to meet the needs of sex-trafficked and exploited young people through age 24. Under Minnesota’s Safe Harbor law, sexual exploitation and sex trafficking victims and survivors are protected from criminal prosecution and can access Safe Harbor services, including housing. “It’s encouraging to see the positive impact of Minnesota’s Safe Harbor approach, as we at the health department and our colleagues in human services and law enforcement work to address the serious problem of sexual exploitation,” said Minnesota Commissioner of Health Dr. Brooke Cunningham. “The youth who participate in Safe Harbor services are resilient and want trauma-informed and culturally responsive services that help them reach independence through meeting basic needs, case management and housing.”
A substantial majority (95%) of recent program survey respondents said they were satisfied with the Safe Harbor services they received. Minnesota’s Safe Harbor law went into effect in 2011 and the program launched in 2014. Between April 2021 and March 2023 Safe Harbor enrolled 1,494 survivors in the program. This was an increase over previous three-year-evaluation periods. Despite this encouraging growth, it is clear there are more Minnesota youth and young adults needing help. A University of Minnesota analysis of 2022 data estimated at least 4,800 high-school-age youth in Minnesota had traded sex or sexual activity for money, food, drugs, alcohol, a place to stay or other reasons. Safe Harbor reported the average age of sex-trafficking survivors it served was 18. A higher percentage of youth served were in Greater Minnesota with 63% compared to the metro area with 37%; 77% of survivors were female, 11% identified as male and 12% as transgender, gender non-conforming and other. For more information visit the Safe Harbor Minnesota webpage.
Free Insulin Now Available Across Minnesota
Following a settlement resolving the 2018 lawsuit filed by Minnesota Attorney General Keith Ellison against Eli Lilly, his office recently announced free insulin is now available in several Minnesota clinics. Six more clinics in Minnesota are yet to be selected to provide free insulin. In addition, all Minnesotans, with or without insurance, can buy Eli Lilly’s insulin products for $35 per month for the next five years. Attorney General Ellison reached a similar settlement guaranteeing $35 per month insulin with Sanofi on July 23, 2024. Working with Direct Relief, a nonprofit humanitarian organization whose mission is to improve the lives of people in poverty or emergency situations, nine Minnesota clinics have signed up for free insulin donations. The free insulin program is intended for low-income Minnesotans and requires specific eligibility criteria, which are determined by the clinics and the applicable charitable organization. “If you need insulin to survive, you should be able to get that insulin. Period,” Attorney General Ellison said. “I am pleased and grateful that Minnesota clinics and Direct Relief have stepped up to coordinate distribution of this life-saving medication to people who might not otherwise be able to pay for it. I will continue to do everything in my power to help Minnesotans afford their lives, and that includes affording the medicine that keeps them alive.”
The Minnesota clinics approved so far for distribution of free insulin are:
- Scenic Rivers Health Services
- Lake Superior Community Health Center
- Hennepin Healthcare System
- Indian Health Board of Minneapolis, Inc.
- Southside Community Health Services, Inc.
- C.A.R.E. Clinic
- Minnesota Community Care
- St. Mary’s Health Clinics
- United Family Medicine
“There are still opportunities for six more clinics to receive free Eli Lilly insulin for their patients,” Attorney General Ellison continued. “If you’re a clinic already doing the hard work of making sure people are healthy in your community, talk to us, let’s work together to expand free insulin access to Minnesotans across the state.” Clinics interested in participating in free insulin distribution should contact the Attorney General’s office at insulin@ag.state.mn.us.
MORE STORIES IN THIS ISSUE
cover story one
Assessing and Advancing Community Health: The overarching value of equity
By Brooke Cunningham, MD, PhD
cover story two
Generation Alpha and Skincare: Health care impact of a new craze
By Sheilagh Maguiness, MD
capsules
Top news, physician appointments and recognitions
Interview
A New Name for an Unchanged Mission
Rachael Perlinger is president of Healthcare Leaders Association of Minnesota and clinic administrator at Northland Plastic Surgery in Duluth
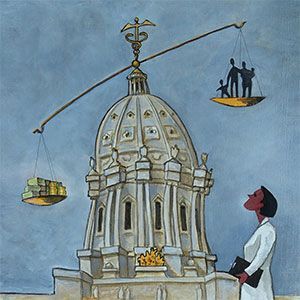
Health Care Roundtable
Health Care Reimbursement Transparency: Inside the black box
AUGUST 2024
cover story
Assessing and Advancing Community Health: The overarching value of equity
BY Brooke Cunningham, MD, PhD
CONTACT
(612) 728-8600 | comments@mppub.com
758 Riverview Ave | St. Paul MN 55107
© Minnesota Physician Publishing · All Rights Reserved. 2023
quick links
We welcome the submission of manuscripts and letters for possible publication. All views and opinions expressed by authors of published articles are solely those of the authors and do not necessarily express those of Minnesota Physician Publishing Inc., or this publication. The contents herein are believed to be accurate but are not intended to replace medical, legal, tax, business or other professional advice or counsel. No part of this publication may be reprinted or reproduced without written permission from our publisher.