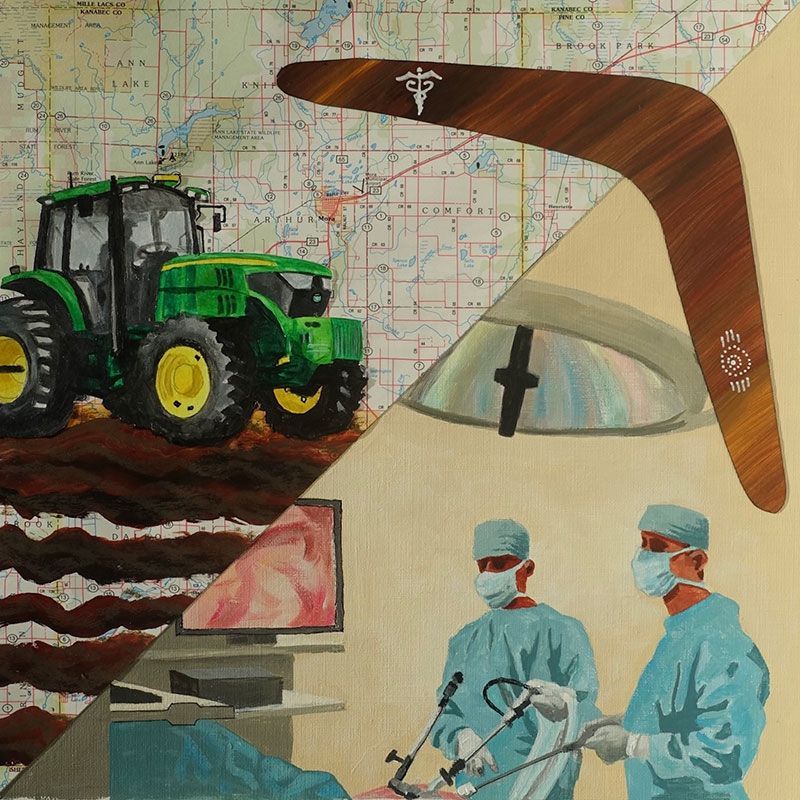
silent crisis is unfolding across America’s heartland, threatening not just rural communities but one of the nation’s most vital economic engines. Beyond the headlines of supply chain disruptions and food security lies an even more pressing challenge: rural Americans are increasingly cut off from the advanced medical care that their urban counterparts take for granted. The challenge stems from a fundamental mismatch between medical economics and rural realities. Advanced procedures such as minimally invasive surgeries require both sophisticated equipment and sustained clinical expertise—typically hundreds of cases annually to ensure optimal outcomes and justify substantial investments. Rural populations lack the critical mass needed to sustain advanced medical programs. This scarcity of patients creates a two-fold challenge: specialized centers can’t justify the large investments in equipment and infrastructure, while subspecialists face professional isolation and skill degradation without adequate case volumes. For rural patients, the consequences are stark. Those needing urgent advanced procedures must either travel hundreds of miles to urban centers—assuming they have the means—or settle for dated surgical techniques available locally. A farmer with a complex gastrointestinal tumor, for instance, might face a choice between a six-week wait for minimally invasive surgery in Minneapolis or immediate open surgery at a local hospital, with its higher risks and longer recovery times.
Cover one
Maps of Healing:
Rural Horizons of Tertiary Care
BY Fateh Bazerbachi, MD
CentraCare, a Minnesota-based health system, is piloting what could be a blueprint for rural health care delivery. Operating from St. Cloud, a city of 70,000 that sits at the intersection of the state’s farming belt and its metropolitan core, the system has developed a hub-and-spoke model recently described in the Journal of Hospital Medicine. The program’s implementation experience offers health care executives nationwide early insights into a novel approach for rural care delivery. The timing is significant: amid a growing crisis in rural health care access, the model suggests new possibilities for maintaining advanced medical services in agricultural regions.
The approach challenges a long-held assumption in health care economics: that advanced medical procedures can be sustainable only in major metropolitan markets. Initial observations from the program suggest this model might help bridge the growing urban-rural divide while maintaining the clinical volumes needed for quality care.
Rural populations lack the critical mass needed to sustain advanced medical programs.
The Human and Economic Impact
The cost of rural health care gaps becomes starkly clear in cases of early-stage gastrointestinal cancer. Rural patients needing advanced procedures such as endoscopic submucosal dissection face lengthy journeys to urban medical centers, where waiting lists often stretch for weeks. Beyond travel time, these patients confront the additional burden of expensive urban lodging—costs that compound already significant medical expenses.
The economic ripple effects extend far beyond individual farms. Modern agricultural operations, managing thousands of acres with minimal staff, prove particularly vulnerable when key personnel must travel for medical care. These absences affect critical decisions about labor management, equipment deployment, irrigation timing and harvest scheduling. During peak seasons, such disruptions create operational bottlenecks that diminish regional productivity and can influence market dynamics.
These access barriers often force patients toward more invasive traditional surgeries, such as colon resections, rather than newer minimally invasive options. This choice, driven by convenience rather than medical necessity, carries serious implications. Surgical complications such as anastomotic leaks or strictures can lead to prolonged recovery periods and multiple follow-up procedures. Beyond the immediate impact on patients, these complications strain health care resources, requiring extended hospital stays, additional procedures and intensive follow-up care. The cumulative cost of managing these complications typically far exceeds that of minimally invasive alternatives, creating an unnecessary burden on an already stressed rural health care system.
Rural Health Care as National Security
America’s Upper Midwest is emerging as a cornerstone of global food security at a pivotal geopolitical moment. While traditional agricultural powers falter—China faces depleting aquifers, Brazil confronts demographic challenges, Russia experiences population decline and Ukraine’s farming capacity remains war-disrupted—America’s heartland stands uniquely positioned to meet growing global demand.
The region’s natural advantages tell part of the story. Fertile soil, reliable rainfall patterns and the Mississippi River’s transportation network create an unmatched agricultural infrastructure. These assets grow more valuable as developing nations across Asia and Africa shift toward protein-rich diets, transforming the Midwest’s grain production capacity from regional strength to global strategic asset.
But this potential rests on a critical foundation: maintaining viable rural communities with sophisticated health care infrastructure. When agricultural producers must choose between accessing advanced medical care and maintaining operational continuity, it creates vulnerabilities in one of America’s most strategic economic engines. The ability to deliver specialized medical procedures locally thus transcends health care policy—it becomes a matter of national strategic interest, directly tied to America’s capacity to ensure global food security and maintain its position as a leader of the free world.
As global food markets evolve and geopolitical tensions rise, these agricultural advantages position the region as an increasingly vital player in maintaining global food stability. However, this potential can be fully realized only with robust local health care systems that keep agricultural operations running efficiently.
A Three-Pronged Revolution
St. Cloud Hospital has upended traditional rural health care delivery through an integrated system that brings metropolitan-level care to America’s heartland. The approach recognizes that rural health care needs fall into distinct categories, each requiring targeted solutions while preserving crucial doctor-patient relationships.
Outpatient Routine Care: The Hub-and-Spoke Evolution
The system’s core innovation lies in delivering sophisticated procedures—from complex endoscopic mucosal resection to specialized pancreatobiliary treatments—previously confined to major cities. By establishing a regional hub, the hospital maintains the high procedure volumes essential for clinical excellence while serving a broad rural area.
The hub’s foundation rests on a state-of-the-art advanced endoscopy unit equipped with dedicated anesthesia support and cutting-edge equipment matching that of major academic centers. This investment ensures that rural patients access sophisticated procedures with the same technical capabilities found in metropolitan hospitals.
The model goes beyond procedure delivery. Through partnerships with local health care systems, patients complete pre-procedure work at their community facilities. Virtual consultations eliminate unnecessary travel. This approach keeps primary care physicians central to patient care, with specialists serving as integrated partners rather than distant consultants.
Hospital leadership has backed this vision with infrastructure investments, including specialized nurse navigators and care coordinators dedicated to advanced endoscopy. These professionals orchestrate complex care pathways from pre-procedure preparation through post-procedure follow-up, delivering sophisticated care without sacrificing the personal touch essential to rural medicine.
The Boomerang Program: Reimagining Urgent Specialized Care Delivery
The Boomerang (Round-Trip) Program represents a paradigm shift in specialized urgent care delivery for rural communities. This same-day, round-trip service allows rural hospitals to maintain their essential role in patient care while accessing advanced procedures typically limited to major medical centers.
The program elegantly addresses a critical challenge in rural health care delivery: providing sophisticated interventional procedures without disrupting local care systems. When patients require specialized interventions but don’t need extended stays, or when bed capacity is limited, the program enables rapid transfer for specific procedures, followed by immediate return to local hospitals for recovery and ongoing care. This approach preserves critical access hospital beds, maintains continuity of care and strengthens local health care infrastructure.
The program’s success relies on robust staffing and sophisticated coordination. The hospital maintains consistent daily service, including weekends, through appropriate staffing levels and support infrastructure. The core charge nursing team manages complex logistics, from medical record transfers to interfacility communication, proving particularly effective for time-sensitive cases like acute gastrointestinal bleeding and pancreatobiliary emergencies.
The Gorecki Guest House Initiative
Health care access in rural America faces a challenge that extends beyond medical capabilities: the logistical and financial burden of accessing specialized care. The Gorecki Guest House provides an innovative solution by offering affordable accommodation directly across from St. Cloud Hospital. This strategic positioning addresses a critical gap that major urban centers often overlook. While metropolitan hospitals frequently offer advanced procedures, they rarely account for the complete patient experience, leaving rural residents to navigate expensive hotels, complex parking arrangements and unfamiliar urban environments.
The facility’s impact extends beyond convenience, playing a vital role in clinical outcomes. For example, clinical data demonstrate that patients traveling more than 30 miles for procedures often struggle with adequate colonoscopy preparation, a crucial factor in procedure success. The Gorecki Guest House’s proximity enables optimal procedure preparation while maintaining cost accessibility, particularly important for our third-space endoscopic resection program.
The initiative strengthens rural economic resilience by removing both logistical barriers and financial strain, enabling more rural residents to access specialized care with minimal disruption of their work and family responsibilities. This comprehensive approach to patient support demonstrates how health care innovation must extend beyond clinical capabilities to address the full spectrum of rural health care challenges.
Many advanced endoscopic procedures and specialized tools lack specific billing codes.
A Robust Operational Framework
Behind our rural health care innovation lies a precisely engineered operational system. The model runs on a dual-team structure: from 8 a.m. to 4 p.m., fellowship-trained interventional endoscopists handle complex procedures including endoscopic submucosal dissection and therapeutic ultrasound. The 4 p.m. to 8 a.m. shift transitions to GI hospitalists managing urgent cases such as bleeding and foreign body removal.
The system maintains flexibility beyond standard hours. Emergency cases bypass typical admission protocols, moving directly to operating rooms when needed. ICU teams stand ready for critical cases such as variceal bleeding. For urgent but non-immediate cases such as cholangitis, the GI hospitalist team coordinates next-morning procedures through structured handoff protocols.
A central transfer center serves as the system’s nerve center. Rural providers connect directly with nursing supervisors and medical officers to initiate specialized procedure consultations. The program accommodates same-day procedures even during high hospital occupancy periods—a crucial capability for rural health care delivery.
The model builds in multiple safety checkpoints. Referring facilities must secure admission beds for patient returns before transfers begin, preventing potential displacement during shift changes. The endoscopy unit follows specific protocols for pre-procedure requirements, coordinating with originating hospitals for necessary labs and workups. Multiple review layers, including final anesthesia team approval, precede patient transport.
The system embraces technological practicality. While facilities using Epic’s CareEverywhere platform share records electronically, those without integrated systems can send physical imaging media with patients. This flexibility ensures all facilities can access specialized care regardless of their technical infrastructure.
Quality metrics drive continuous improvement. The program tracks transfer times, procedure outcomes and return-to-facility success rates. A key indicator—the attrition rate measuring unexpected admissions—evaluates pre-procedure screening effectiveness and care setting selection accuracy.
Beyond immediate care coordination, the program maintains ongoing dialogue with rural providers, enhancing their ability to identify cases suitable for advanced endoscopic intervention. This educational component strengthens the regional health care network and improves early identification of cases requiring specialized care.
Case Studies
St. Cloud’s rural health care model demonstrates how innovative medical approaches preserve both health outcomes and economic vitality in America’s heartland.
The system’s impact emerges clearly in complex cases. A middle-aged farmer facing a large circumferential rectal tumor—traditionally requiring major surgery and permanent colostomy—instead received endoscopic submucosal dissection (ESD). Drawing on expertise developed through nearly 400 advanced resection cases, the team achieved complete tumor removal without major surgery, enabling next-day return to agricultural operations.
Strategic partnerships proved crucial in transforming outcomes for a young commercial truck driver with life-threatening necrotizing pancreatitis. Through weekly virtual case reviews with University of Minnesota colleagues and industry partnerships providing powered endoscopic debridement technology, the team converted a potentially fatal diagnosis into a manageable two-month recovery, preserving another vital link in rural America’s supply chain.
The system’s capacity for complex care while maintaining cultural sensitivity emerged in treating a young immigrant with a severed bile duct. Through integrated interventional radiology and advanced endoscopy, while meeting cultural and linguistic needs, the team achieved a minimally invasive solution avoiding complex surgery.
Rural surgical capabilities reached a new milestone with a groundbreaking combined endoscopic-laparoscopic procedure using Submucosal Tunneling Endoscopic Resection (STER) for a large gastrointestinal tumor. This organ-sparing approach preserved crucial nerve function. When faced with extraction challenges, the team’s adaptability enabled swift transition to laparoscopic removal. The patient’s 24-hour discharge demonstrated rural health care matching metropolitan standards while maintaining community accessibility.
These cases represent more than medical successes: they demonstrate how technical innovation, strategic partnerships and human-centered care delivery strengthen rural economic resilience and community sustainability.
Challenges and Future Directions
In his seminal work “Prisoners of Geography,” Tim Marshall explores how physical barriers—mountains, rivers, deserts—have historically constrained human development and shaped nations. Today’s rural health care faces similar geographic constraints, but two fundamental challenges threaten to reinforce these barriers: transportation infrastructure limitations and inadequate reimbursement for advanced medical services. Current health care policies, designed primarily for urban settings, create operational hurdles that endanger emerging care systems.
The EMS challenge illustrates this policy misalignment. County-level jurisdictional boundaries frequently disrupt efficient patient movement, particularly across multiple service areas. While Medicare and private insurers cover emergency hospital transport, they often restrict coverage for returning stable patients to local facilities. This reimbursement gap strains rural emergency medical services, which must maintain full staffing and equipment readiness despite uncertain payment for essential transfers.
Retaining specialized medical expertise in rural areas presents another market challenge. Unlike urban centers supporting multiple specialists, rural areas struggle to maintain advanced medical capabilities. Current health care policy provides limited incentives for specialists to practice in rural settings. Solutions require expanding loan forgiveness programs, adjusting reimbursement rates to reflect rural practice challenges and supporting continuing education programs.
Most critically, medical coding and reimbursement systems lag behind health care innovation. Many advanced endoscopic procedures and specialized tools lack specific billing codes, forcing providers to use inappropriate or inadequate codes that don’t reflect true care costs. This misalignment particularly impacts rural centers, where lower patient volumes make it difficult to absorb specialized equipment costs.
Whereas Marshall portrayed the immutable forces of topography—towering mountains, turbulent seas and unforgiving deserts—as unyielding constraints, in the realm of health care such geographic limitations are being decisively dismantled. Through a potent combination of innovation, strategic partnerships and relentless resolve, we are not merely escaping the confines of geography but actively redrawing the cartography of rural health care. This transformation ensures that even the most remote communities gain timely and equitable access to vital medical services, redefining the relationship between place and care.
Fateh Bazerbachi, MD, is the director of interventional endoscopy at CentraCare - St Cloud Hospital.
MORE STORIES IN THIS ISSUE
cover story one
Maps of Healing: Rural Horizons of Tertiary Care
By Fateh Bazerbachi, MD
cover story two
Living with ADHD: Understanding and empowerment