are coordination has great potential to make a difference in the lives of Minnesotans. Many organizations have incorporated the care coordinator role within their business models with the purpose of bringing value and support to the people they serve. These individuals may be assigned to or contacted by a care coordinator (maybe with a different title but with the same purpose) from a variety of organizations connected to their medical or social services: public health, insurance companies or other support agencies. While the actions and work of care coordinators in each setting bring value to the patient, consistent communication and collaboration between all the individual’s care coordinators is a high priority to support them without confusion, reduce duplication of efforts and ultimately improve the patient’s health outcomes while keeping the individual at the center of care.
August 2022
VOLUME XXXVI, NUMBER 05
August 2022, VOLUME XXXVI, NUMBER 05
cover story two
Care Coordination
Improving patient satisfaction and engagement
By Bonnie LaPlante, MHA, RN

In Minnesota, patients receiving primary care services can work directly with a care coordinator in certified Health Care Homes. Minnesota Health Care Homes (HCH) are known nationally as patient-centered medical homes. Most Minnesota’s primary care clinics are certified through the Minnesota Department of Health as an HCH. Certified clinicians and their care teams are changing their way of providing care across the state. Using a care coordinator and a patient-and family-centered approach, they help patients access care in the right place at the right time, navigate through a complex care system, engage in their health care through active decision-making and goal setting and optimize health outcomes and overall population health. It is a proactive approach which contributes to a patient’s well-being.
Care coordinators organize patient activities and share information with all members of the patient’s health care team to achieve safer and more effective care. Services are high touch and build a strong relationship between the patient, primary care clinicians and their care team. In Minnesota, certified primary care clinicians have embraced voluntary certification, combined with technical assistance and structured learning opportunities, to drive quality improvement (QI) and transformation in their clinics. The HCH approach shifts the clinic’s or health system’s focus from responding to patient’s needs to proactively engaging a population of patients and focusing on their health goals, needs and abilities to achieve desired health outcomes. The model encourages using the expertise of all members of the care team, including patients and their families.
To be certified, a primary care clinic must demonstrate that it has met standards in the five domains of access and communication, registry and tracking, care coordination, care planning and performance reporting and quality improvement, each with specific criteria. Standards and criteria reflect the main goals of the program: to recognize individual patients and families as the most important part of the care delivery process and to put systems and processes into place to improve patients health outcomes.
Care coordination needs vary among populations and individuals.
In primary care, care coordination needs vary among populations and individuals. Some care coordination processes are provided to the clinic’s entire attributed population by various members of the health care team, using appointment reminders, notification of gaps in care, transition of care support, coordination of specialty referrals, appointment follow-up support, and medication reconciliation. For emerging risk, high-risk and high-cost individual patients, one-on-one contact with a care coordinator provides “between visit” tracking, follow-up and coaching. This additional support to patients and families facilitates effective care management while allowing primary care providers to work at the top of their license. Intensive, one-on-one care coordinator patient support can improve health outcomes for individual patients with complex needs. Holistic and ongoing longitudinal support helps patients and/or their designated family member find the best approach to managing care needs, establish short term achievable goals to improve current health concerns, prevent worsening of health conditions and access health care at the right place at the right time. The care coordinator in primary care helps patients manage their conditions and navigate a complex medical care system. Care coordinators have strong knowledge of the entire care system and can simplify processes to guide and help a patient understand and make their way through a complex system. They communicate effectively with providers to ensure patients get the information they need to make informed decisions about their personal health care needs.
Engaging the Patient
Developing a care plan and providing self-management education is particularly important for patients with chronic diseases and emerging modifiable risks. There are a variety of resources to meet patient needs, and one size does not fit all. The care plan starts with a comprehensive assessment that provides insight into the medical and non-medical needs of the patient. The assessment is used to inform the care plan with patient-centered goals that address health and wellness gaps. A patient-centered approach includes providing care that is respectful of and responsive to individual patient preferences, needs and values, while ensuring that patient values guide all clinical decisions. Using a patient-centered approach improves patient satisfaction and engagement.
Improving Patient Outcomes
Care coordination in primary care is more effective when the patient is engaged and participating in their care. Care coordinators can help patients engage by understanding individual patient activation levels (knowledge, skills and confidence to manage one’s health) and meeting them where they are. Using evidence-based tools and techniques such as motivational interviewing, self-management education programs, setting patient-centered goals and tracking progress towards goal attainment—all foster individuals’ self-management of their medical conditions.
Another potential benefit of effective care coordination is the facilitation of appropriate care within and across health care systems and the community. Care coordinators help patients, and their families access the system at the right time and right level of care before a higher level of care is required. Helping patients and their families to be successful in self-care and proactive care management can reduce the cost of care by preventing avoidable emergency room visits and hospitalizations.
Patients receiving intensive care coordination often need to see multiple health care providers and require various procedures. Some also have unmet social needs. A care coordinator focuses on the whole person since there are many factors outside of a patient’s clinical condition which impact their health and well-being. For patients with complex medical and social needs, care coordinators can help patients address social barriers such as food insecurity, access to transportation for medical appointments, affordability of medications, housing and insurance coverage by making and following up on referrals to community organizations.
Primary care providers are key collaborators in the care coordination process. They facilitate warm hand-offs to the care coordinator, speak about the care coordinator as an extension of the care team, communicate with patients in a way that aligns with the care plan and maintain close working relationships and effective communication with the care coordinator.
Primary care providers are key collaborators in the care coordination process.
Who Should be a Care Coordinator?
In Minnesota, individuals working in the role of care coordinator come from different backgrounds with variation in educational training, licensure, discipline and expertise. Successful care teams may have individuals with a variety of qualifications serving as a care coordinator. Care coordinators may be a Registered Nurse (RN), Licensed Practice Nurse (LPN), Certified Medical Assistant (CMA), Community Health Worker (CHW) or a Social Worker (SW). This variety of roles allows primary care organizations to tailor the composition of their team to meet the medical, social and cultural needs of the populations they serve. Variation of training and licensure within a care team can allow organizations to develop systems that optimize their resources, allowing care coordinators and other members of the team to function at the top of their licensure, supporting strong teamwork and improving the job satisfaction of each member of the team.
Understanding the clinic’s target population provides the best solution to meeting patient needs and selection of a care coordinator. The care coordination scope of practice, training, tools and resources support the care coordination model best when matched to the breadth of responsibilities they will manage from a population perspective, creating an environment of success and improved outcomes for the patient.
Understanding race, ethnicity and language, along with health complexity and disease prevalence through a Community Health Assessment, Community Health Improvement Plan, county rankings and/or utilization data can provide insight to the needs of the target population. For example, if a clinic has determined their target population has patients with mental health diagnosis and uncontrolled diabetes, they may be seeking an applicant or existing team member with experience and training in diabetes management and previous work experience in behavioral health.
Professional and workplace skills are often differentiated as soft skills or emotional intelligence in contrast with hard or technical skills. Technical or hard skills can be verified through certifications, degrees and work experiences. Soft skill elements are defined as the ability to connect and communicate, respect differences, work with teams and build relationships to effectively support the needs of the patients served in the targeted care coordination population. Both skill types are very valuable traits in providing care coordination. Evaluation is a critical tool for demonstrating a care coordination program’s impact, assessing effectiveness, determining return on investment, assessing patient satisfaction and identifying future programmatic needs and opportunities. Primary care organizations will want to institute a quality improvement process to ensure program goals are met and patient and program outcomes are evaluated. Quality improvement should focus on both the patient as well as the care coordination processes, considering what matters and to whom the changes will matter, such as clinicians, patients, staff or regulatory bodies.
Care coordination also benefits payer organizations. Payers benefit by reducing fragmented care that results in additional costs and risks to complex patients and wasteful spending on things like unnecessary testing, duplicative procedures and emergency room visits for uncontrolled conditions.
Most payers require providers to demonstrate ongoing quality improvement, patient satisfaction and lower overall cost of care—all achievable goals with a strong care coordination structure. Care coordination at a primary clinic facilitates a strong and cohesive working relationship between all members of the primary care team, the physician and the patient. When all members of the team work together towards shared goals, patients feel engaged and valued. Their care is better understood, becoming more effective and less fragmented. Using a patient-centered approach in turn leads to higher levels of patient wellness and improved health outcomes. It allows physicians and others to work at the top of their license, expands the physician’s reach to optimize a patient’s well-being and meets the goals and objectives of patients, providers and payers.
Bonnie LaPlante, MHA, RN, is the Health Care Home (HCH) Program Director, in the Health Policy Division, at the Minnesota Department of Health.
HCH Patient Story
A care coordinator working with a patient experiencing early cognitive decline recognized the need for family involvement. She reached out to the patient’s son to fill him in on his mother’s condition, and he quickly helped to prioritize safety as their top concern. By working together with the patient and her son, the care coordinator located a home health agency that now sets up medications, takes her to appointments and provides other care during the week.
HCH Patient Story
Clinic staff had identified that a patient was needing to cancel appointments due to an inability to find transportation. Coordination staff worked with the family to understand and assess this barrier and learned that the patient was not able to navigate the process to access their medical transportation benefits due to a language barrier. Staff were able to provide instructions in the family’s own language and walk through the steps with them so that they could now do this for themselves.”
HCH Clinic Manager Comment
Collaborative care plans at Ridgeview took everything we were already doing and put the information down in one location for all the care team to see, including the patient. Finding out what was important to the patient changed our perspective on the care planning process.
HCH Clinic Leadership Comment
Despite the challenges of the pandemic, patients with care coordination at our clinic remained stable and received consistent care throughout COVID. “We are proud of that,” said a leader on the care coordination team. “Care coordination has been a steadying source for many patients when everything else has gone to heck.”
MORE STORIES IN THIS ISSUE
cover story one
The Moral Law Within: Care beyond medical services
By JULIA JOSEPH-DI CAPRIO, MD, MPH
cover story two
Care Coordination: Improving patient satisfaction and engagement
Bonnie LaPlante, MHA, RN
capsules
Top news, physician appointments and recognitions
Interview
Improving the Experience of Health Care
Hilary Marden-Resnik, President and CEO
Medicine and the Law
The Interstate Medical Licensure Compact Commission: Expanding your practice opportunities
BY Marschall S. Smith
Administration
The Minnesota Rare Disease Advisory Council: A new resource for patients and clinicians
BY Erica Barnes, Ma, CCC-SLP
Health Care Policy
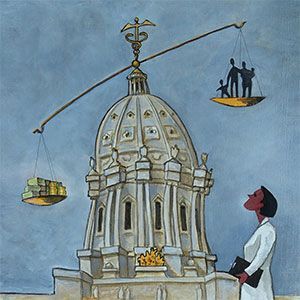
Physician Advocacy: You are needed now
BY PETER DEHNEL, MD
AUGUST 2024
cover story
Assessing and Advancing Community Health: The overarching value of equity
BY Brooke Cunningham, MD, PhD
CONTACT
(612) 728-8600 | comments@mppub.com
758 Riverview Ave | St. Paul MN 55107
© Minnesota Physician Publishing · All Rights Reserved. 2023
quick links
We welcome the submission of manuscripts and letters for possible publication. All views and opinions expressed by authors of published articles are solely those of the authors and do not necessarily express those of Minnesota Physician Publishing Inc., or this publication. The contents herein are believed to be accurate but are not intended to replace medical, legal, tax, business or other professional advice or counsel. No part of this publication may be reprinted or reproduced without written permission from our publisher.