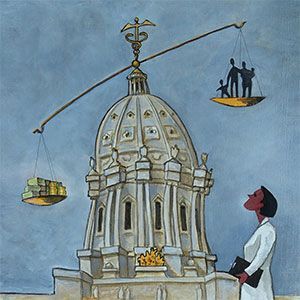
he U.S health care marketplace is at an interesting inflection point, and this time it more specifically implicates career decisions for certain physician subspecialties, especially clinical specialties that operate primarily in the ambulatory care arenas. Particularly implicated are specifically identified clinical service lines (CSLs) that are not wholly dependent upon referring physicians for patients. Successful CSLs operate with effective brand positioning strategies which strive to predetermine patient choice, e.g., the patient has made up their mind where to go for care before the need arises, e.g., “If I get cancer, I’m going to the [xyz] cancer center.” Practical experience demonstrates that referring physicians are not likely to persuade patients to do something other than their expressed choice for specialty care.
January 2022
VOLUME XXXV, NUMBER 10
January 2022, VOLUME XXXV, NUMBER 10
Practice Management
Clinical Service Lines
Reasons people don’t seek help
BY DANIEL K. ZISMER, PhD, GARY S. SCHWARTZ, MD, MHA

Clinical service lines (CSLs)
Before moving forward with the central theme of this article, CSL model decision-making for clinical specialists, it’s useful to begin with a common definition and understanding of a CSL.
A clinical service line is a grouping of related clinical services and programs dedicated to an identified constellation of related diagnoses and conditions, designed to produce and deliver a superior course of care, over time, based upon evidenced-based best practices for defined clinical populations.
Now, back to the inflection point discussion. Specialty CSLs are at the top of the strategies list for three very different models of delivery. Examples of CSL getting the most attention and investment dollars include: orthopedics, cancer care, eye care, heart care, wellness, sophisticated urgent care, behavioral health, industrial medicine, dental care and oral surgery, GI, ENT, urology, a range of pediatric subspecialties and primary care networks. Are there common denominators here? There are a few that make sense, at least when looking through the lens of strategy and finance. All these generate most of earned revenue in the outpatient arenas. The anatomy of the grouped revenue streams include: professional services, imaging diagnostics, interventional procedures and some forms of retail products and services sales. Demographic trends favor future growth in service demand. Moreover, the operating economics available lend well to effective productivity management and targeted strategic investment strategies.
Successful CSLs operate with effective brand positioning strategies.
Three types of CSL organizational designs
The three types of organizational designs operating in and competing for the CSL markets and related rewards include:
- Larger, integrated community health systems.
- Academic health centers.
- Specialized, independent physician groups that consolidate and aggregate subspecialty providers to achieve sufficient size, scale, scope and geographic reach and to attract required levels of investment capital.
All three models can succeed with capable leadership, focus and commitment. The question for the physician specialist is “which model is right for me?” The balance of this article presents a framework for practice option decision-making. First, we consider a brief comparison of the three organizational designs.
The integrated, community health system (IHS)
Typically, the IHS will identify and aggregate a number of related physician specialties and related clinical programming under the system brand; independent and employed providers may be involved in the brand strategy. The IHS typically owns the CSL, including the larger portion of the associated revenue streams. It capitalizes the start-up, and IHS senior leadership oversees operations and performance. Most typically, the IHS operates as a not-for-profit organization under the U.S. Internal Revenue Code. Independent physician groups may become affiliated with the strategy and practice alongside providers employed by the health system. Independent physicians may also enter into for-profit partnerships and joint ventures with IHS service lines, ambulatory surgery centers, for example.
The academic health center (AHC)
The AHC is usually, but not always, university affiliated. They exist to serve a three-pronged mission strategy: teaching, research and clinical care. They may rely upon grant funding for a considerable portion of their total mission budget. Leadership, management and operations financing can be more or less centralized, and interests of clinical departmental leaders can be tipped variously to any one of the three mission paths and related strategies.
The pure play physician model
The pure play model is typically focused on more easily identified and understood brand and mindshare strategies aimed at specific patient markets and clinical services programming, such as orthopedics, cancer care and comprehensive eye care. The organizational and business model is often physician owned and controlled. The pure play models can be wholly capitalized by the physicians who own them, or investment capital can be pooled with for-profit sophisticated investors, private equity players, for example.
Questions to Ask
So how does the specialty physician find the suitable CSL home (i.e., “which model is best for me”?). The issues that follow will provide insight into this question. Consideration of these issues will require some soul-searching, a bit of research and discussion with experienced peers.
- I practice in a specialty that has the potential to take a brand strategy directly to the end user (the patient). Provider referrals are important but are not likely to comprise the larger portion of new patient flow over the course of my career.
- Hands-on physician decision-making control is important to me, i.e., direct physician control over organizational governance, leadership, management, strategy and patient care.
- My specialty requires a close relationship with deep, complex hospital service capabilities, including their ability to make significant investments in clinical technologies and specialized facilities.
- The economics of the payer mix for my specialty must be financially supported by a broader and diverse clinical service portfolio and business model – one that integrates what I do with other more profitable specialty services. In other words, the economics of my specialty are not as favorable as a “stand-alone” CSL
- I am willing to put my own money at risk in the model, i.e., take personal financial risk in hopes of reaping greater financial reward over time.
Pure play models can be wholly capitalized by the physicians who own them.
- In addition to being a clinician, I am interested in a career path that includes freedoms to pursue a range of professional interests: leadership, research, entrepreneurial innovation, teaching or deeper sub-specialization. In other words, my career plans permit me to evolve my career within the model I select.
- I want to help build a business that creates equity for me, i.e, my ownership that has real future financial value potential beyond the compensation I earn.
- The model selected will lend well to the continued recruiting of other high quality providers and staff, even as competition for the best professionals increases.
- Future market-place, reimbursement and operating economic trends portends more positively or negatively for my specialty.
- Well-capitalized competitors will be investing heavily in the services delivered by my specialty, including select related ancillary services opportunities.
Characteristics of successful CSLs
Whether delivered by way of any model described above, successful CSLs share common characteristics. The characteristics described here derive, in-part, from the specialty physician decision-making framework described above. Characteristics of successful CSLs include:
- The brand strategy clearly and effectively positions and differentiates the range of services and CSL value propositions in the mind’s eye of the target end-users: patients, families, referral sources, related community agencies, and targeted market social media communities. Clear, crisp brand strategies emove any market confusion around the “business” the CSL it is in.
- All who serve the CSL (providers and staff) understand the mission of the CSL (its reason to exist), its vision (where the CSL is going and why), along with its strategy the path to achieve stated goals, i.e., how we expect to execute on the mission.
- There is a common and well-known CSL performance scorecard: one available for all providers and staff to see, understand and learn from, especially metrics pertaining to the patient and referring provider experience.
- There is a clear, accessible “front door”, meaning the potential user knows how to effect that first contact, whether as a patient, a family representative or a referring provider.
- Care navigation begins with the first contact. The CSL reaches out, invites the patient in and begins the care management process with the first contact.
- Leaders decide, define, deploy and direct the expected culture of the organization Patients, families and referral sources will gauge the quality of care and the patient experience, as much by the performance of the perceived culture as the clinical outcomes derived.
- The patient identifies with a care team and feels the value of the team regardless of location or service accessed, e.g., the patient is recognized, known and welcomed by staff across sites. Members behave as a cohesive, dedicated, integrated team.
- Services that compose the CSL portfolio are managed to create the financial performance required to achieve the vision and growth strategy defined, including sufficient financial “staying power”.
- The CSL is sufficiently connected to other providers, as needed, to complete the service capabilities and experience promised to the end users.
- Leadership is in a constant state of staff and organizational development in service to the mission.
Putting it into practice
There is a lot of good news here for the clinical specialty providers looking for the right practice platform and environment, providing they pay attention to the market dynamics around them and are prepared to evaluate where they best fit. The risk here is the proverbial square peg in the round hole, i.e., right physician in the wrong model.
The market dynamics that portend CSL strategies can be seen coming. They include: provider-side market consolidation, specialty-related practice acquisitions, mergers and private equity investors acquiring and aggregating specific clinical care provider groups, e.g., orthopedists, cancer specialists, ophthalmologists, etc. Also watch for emerging specialty-based brand positioning strategies in the media and examine organizational recruiting strategies, especially for organizations with known brands, health systems for example. Pay attention to compensation and benefits plans floated by those doing the recruiting, sharp increases, for example. Look for signs of increasing local and regional competition for providers and specialized staff. Finally, use the decision-making framework provided as a guide to determine where you might best fit. Then as you start down the path to deciding with whom or which model type to affiliate, use the list of CSL success factors as a guide as you interview the candidates for your next position.
Daniel K. Zismer, PhD is Co-Chair and CEO of Associated Eye Care Partners, LLC. He is also Professor Emeritus, Endowed Scholar and Past Chair, School of Public Health, University of Minnesota.
Gary S. Schwartz, MD, MHA is Co-Chair and Executive Medical Director of Associated Eye Care Partners, LLC. He is also President of Associated Eye Care Holdings, LLP and Associate Professor, Department of Ophthalmology, University of Minnesota.
MORE STORIES IN THIS ISSUE
cover story one
Health Care Supply Chain Dynamics: Finding room for improvement
By Luis Valadez
cover story two
Medicare Advantage Overpayments: An unsustainable future
By Kip Sullivan, JD
Practice Management
Clinical Service Lines: Which model is right for you?
BY DANIEL K. ZISMER, PhD, GARY S. SCHWARTZ, MD, MHA
capsules
Top news, physician appointments and recognitions
Pediatrics
Treating Pediatric Injuries: What happens in the ice and snow
BY ALLYCE FISK, PA-C, MMS, REBECCA ROUSE, PT, DPT
men’s health
Circumcision: The debate of medical necessity
By Duong Tu, MD
Interview
Improving the Health of All People
Lisa Shannon, CEO Allina Health
AUGUST 2024
cover story
Assessing and Advancing Community Health: The overarching value of equity
BY Brooke Cunningham, MD, PhD
CONTACT
(612) 728-8600 | comments@mppub.com
758 Riverview Ave | St. Paul MN 55107
© Minnesota Physician Publishing · All Rights Reserved. 2023
quick links
We welcome the submission of manuscripts and letters for possible publication. All views and opinions expressed by authors of published articles are solely those of the authors and do not necessarily express those of Minnesota Physician Publishing Inc., or this publication. The contents herein are believed to be accurate but are not intended to replace medical, legal, tax, business or other professional advice or counsel. No part of this publication may be reprinted or reproduced without written permission from our publisher.