October 2022
VOLUME XXXVI, NUMBER 07
October 2022, VOLUME XXXVI, NUMBER 07
cover story one
Mending a Racket
Empower-Patient Accounts
By Robert Koshnick, MD, FAAFP
There is a lot broken in our health insurance system. Health care costs in the U.S. are far higher than the rest of the world. Most people agree this is a problem. Health care went from 5 percent of the gross domestic product (GDP) in 1960 to 19.7 percent in 2020. These costs put a strain on the financial security of individuals and businesses as well as being the primary driver of our federal budget deficits. Our country is less competitive in producing and marketing goods and services in the global marketplace because of the excessive cost of health care.
cover story two
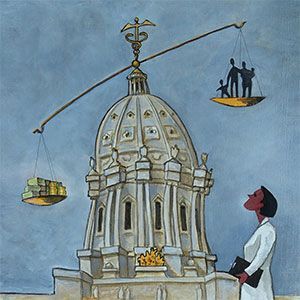
Prior Authorization: The time is now for reform
BY ERIN HARTUNG, JD
Prior authorization is a process almost every physician has dealt with, and often it is not a pleasant encounter. When a health insurance company must approve or deny a service or item before it is provided to the patient, there are many fundamental problems. Prior authorization is supposed to be a method of regulating health care costs and making sure that services are medically necessary. But it often creates unnecessary burdens on health care providers and barriers to important and timely care for patients.
Pain Management
Chronic Pelvic Pain Management: Improving quality of life
BY ERIN BETTENDORF, MD
Chronic pelvic pain can be a life-altering condition which involves physical discomfort and significant emotional stress. While it is widespread among women—in fact, the second most common complaint in gynecologic practice—it can affect men as well. Patients may describe pain as severe and steady or intermittent with symptoms which include dull aching, burning, sharp pains, cramping or pressure and heaviness deep within the pelvis. Pain may be noted during intercourse, a bowel movement or urinating, or when sitting for long periods of time.
Women’s Health
Menopause in 2022: Addressing a knowledge gap
BY Rachel Cady, MD, FACOG, NCMP
The North American Menopause Society (NAMS) 2022 annual meeting opened with a prophetic statement from an acclaimed speaker: “ A tsunami is coming.” Being that the conference was in a landlocked location, I wasn’t literally alarmed but nevertheless intrigued. The “tsunami” was explained to be in reference to the US aging population. The rapidly changing demographic of the postmenopausal population is nothing short of astounding and carries with it immediate implications to clinical care.
Rural Health
Outstate Community Health Resources: Helping patients close to home
BY Hailey Baker and Mahtahn Jenkins
While one in five Americans call rural communities home, only one in ten physicians currently practice in rural communities. Like most states, Minnesota faces challenges maintaining an adequate health care workforce in its rural areas, a situation that has only become worse as a result of the COVID-19 pandemic. According to the Minnesota Department of Health, only 10% of licensed health care workers in our state care for rural Minnesotans, even though 40% of Minnesotans live in rural areas.
AUGUST 2024
cover story
Assessing and Advancing Community Health: The overarching value of equity
BY Brooke Cunningham, MD, PhD
CONTACT
(612) 728-8600 | comments@mppub.com
758 Riverview Ave | St. Paul MN 55107
© Minnesota Physician Publishing · All Rights Reserved. 2023
quick links
We welcome the submission of manuscripts and letters for possible publication. All views and opinions expressed by authors of published articles are solely those of the authors and do not necessarily express those of Minnesota Physician Publishing Inc., or this publication. The contents herein are believed to be accurate but are not intended to replace medical, legal, tax, business or other professional advice or counsel. No part of this publication may be reprinted or reproduced without written permission from our publisher.